Severe facial and eye (orbital) bone deformities and defects may be present at birth or can occur following facial trauma or, most commonly, facial tumor removal. Surgery to correct such defects aims to restore the original anatomy and the patient’s appearance by inserting an implant made either of the individual’s own bone and tissue or synthetic materials. The traditional use of implant materials in facial reconstructive surgery, which are shaped during surgery, often do not recreate ideal three-dimensional contours in the face and take a lot of time working with them as the patient is asleep. Designing synthetic implants beforehand improves theirprecision and contours and helps shorten the time of surgery.
I have looked at my series of ten facial reconstructive patients done over the previous nine years who received computer designed and generated custom implants and were more than one year after their surgery. The six men and four women were between the ages of 31 and 67 years, with an average age of 46.1 years. The defects were caused by either trauma (2), tumor resection (6), or a congenital deformity (2). Most of the patients (7) had a history of prior failed reconstructive efforts. The patients underwent three-dimensional high-resolution CT scanning of the face from which customized implants composed of either pure titanium (bone fixation device) or HTR (porous hard tissue replacement bone substitute) were made. All implants was surgically placed and fixed using titanium plates and screws.
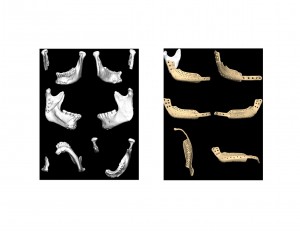
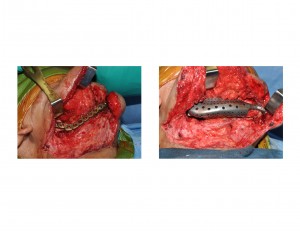
This 62 year-old female had a right mandibular angle bone resection secondary to an intraoral carcinoma. She never had any radiation treatments. The defect was only spanned by a reconstruction plate which had fractured three separate times over the past eight years. A 3-D CT scan showed the defect and the mandibular segment contraction. She did not want a fibular free flap reconstruction.
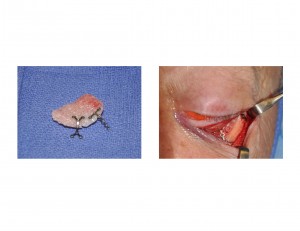
This 65 year-old male had a history of esthesioneuroblastoma with a resection by frontal craniotomy and removal of his left heminasal cavity and maxillectomy. He received radiation afterwards. Over the enduing ten years, he developedorbital floor bony resorption due to osteomyelitis and dropping of the eye downward. His orbital condition and eye position eventually stabilized as his osteomyelitis resolved. A 3-D CT scan shows the loss of orbital floor bone and the orbital dystopia.
During an average of over four years of follow-up, none of the patients experienced any implant-related complications including infection, extrusion, or displacement of the implants. Healing around the implant sites was uneventful. All of the patients had sustained improvement of facial deformities including mouth opening in those that involved the lower jaw.
While numerous types of implant materials have been used for reconstructive facial surgery, one important aspect of their success is proper design and engineering. Time spent before surgery evaluating the exact dimensions of the bone defect and then custom designing the implant has numerous advantages. Having an implant that is not bigger or oversized for the defect lowers the risk of potential extrusion. A near perfect fit makes for good facial contour restoration. Oral function and occlusion is more assured if the lower jaw reconstruction is as precise as possible. Donor site pain and morbidity is eliminated or reduced with maximal use of synthetic replacement parts. Operative times can be reduced significantly, often cutting the length of an operation in half. Implants are also structurally stable and will not resorb or change their shape over time. Any synthetic implant no matter how well designed and engineered, however, has limitations. Good healthy soft tissue flaps over the synthetic reconstruction is extremely important to avoid potential infection and exposure problems.
Dr. Barry Eppley
Indianapolis Indiana