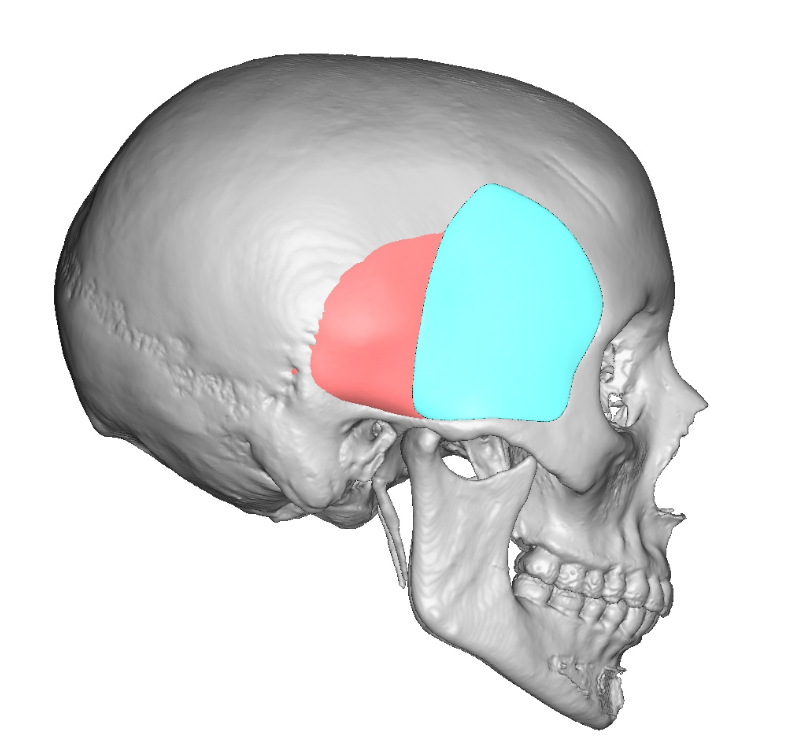
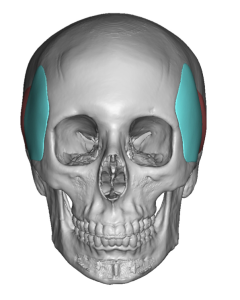
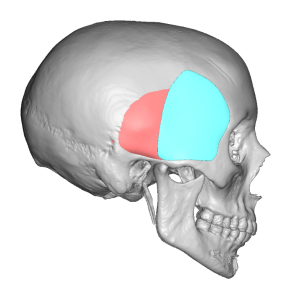
Background: The temples are an aesthetically important region that is separate from the forehead above it and the cheeks below it. While the temporal region anatomically extends from the side of the forehead all the way to the back of the head, the most aesthetically recognized temporal region is anterior by the side of the eye. This very recognizable temporal region is defined by the bony temporal line of the forehead superiorly, the lateral orbital rim anteriorly, the zygomatic arch inferiorly and the more variable temporal hair bearing area posteriorly.
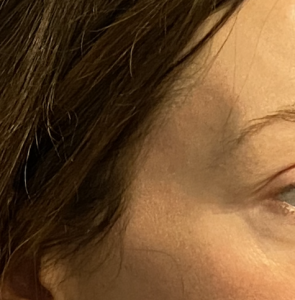
The temples are an often unnoticed facial areas unless a major change in its contour shape occurs. Aging most commonly causes a hollowing of the temples due to fat loss. While everyone will develop temporal hollowing if they live long enough, some men and women develop it much earlier. Barring any medical condition or drug use that is known to cause facial fat loss, why this occurs at younger ages is not known. In my experience and observation thin females are more prone for it to occur.
The aesthetic treatment of temporal hollowing is most commonly done by injectable techniques. Synthetic fillers are the most frequently used due to being an non-surgical method. Fat injections can also be successfully used and is often done as part of other facial surgeries. The injection methods have their distinct advantages but when one seeks assured permanent volume and a smooth contour temporal implants are available. Whether standard temporal implants will work or whether a custom design is more beneficial depends on the amount and extent of the temporal concavity that is present.
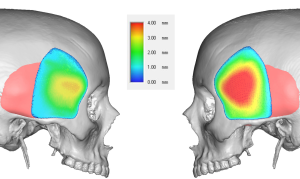


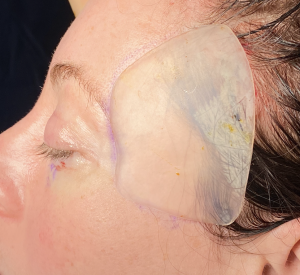
The permanent solution to temporal hollowing is an implant. Implant materials have been used for temporal hollowing over the years but have been fraught with numerous problems. Implants have been placed in the subcutaneous plane of the temporal region but this almost always causes implant show or a visible outline of the implant. Bone cements have been placed deep into the temporal fossa below the muscle but this requires long temporal incisions and irregularities and asymmetries contour issues are not uncommon. Contemporary temporal implants have been developed that have the characteristics of most other successful facial and body implants in which small incisions are used through which pass a deformable implant material that can resume its natural shape once successfully inside the pocket. The real key, however, is the subfascial implant pocket. Placing it under the fascia prevents implant show even though it is on top of the muscle.
Case Highlights:
1) While temporal hollowing affects both women and men, thinner females seem to be more susceptible to age-related fat loss in the temples.
2) Custom temporal implants are indicated when there is temple asymmetry in the concavity seen or when the needed coverage area is bigger than what standard temporal implants cover.
3) A small high hairline temporal incision can be used for their placement despite the mismatch between the size of the implant and that of the incision.
Dr. Barry Eppley
Indianapolis, Indiana