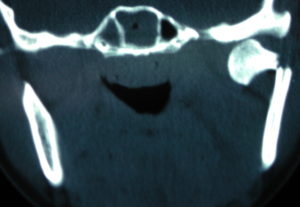
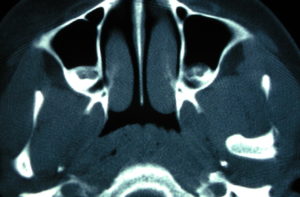
Background: One of the most common facial bone fractures is that of the lower jaw. The mandible is the second most frequently seen facial bone fractures behind that of the nose. It can be fractured at six different locations along this long facial bone and multiple (bilateral) fractures are common. One area of the lower jaw that is particularly prone to fracture is that of the subcondylar region Known as the neck of the jaw joint (TMJ), it is the thinnest section of the entire lower jaw as it supports the condyle above it which sits in the glenoid fossa.
Because it is a thin section of bone that is vertically oriented trauma to the lower jaw, particularly from falls where the force is transferred up along he vertical ramus causes a subcondylar fracture. While subcondylar fractures can occur in isolation, they are more commonly seen with fractures along the jawline on the opposite side of it. If the fall occurs directly on the chin bilateral subcondykar fractures can occur.
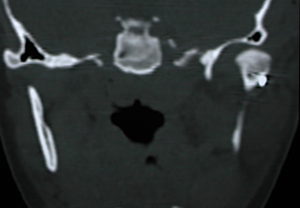
Because of the strong ligamentous attachments to the subcondylar area, most subcondylar fractures keep the condyle within the joint space. As a result closed reduction of these common types of subcondylar fractures is all that is needed. (realigning the lower jaw by occlusal interdigitation fro a short period of time) But when the condylar segment is severely angulated (90 degrees) it becomes entrapped and closed reduction techniques will not get it properly aligned or even close. Open reduction and internal fixation is needed in which the surgical approach depends on the level of the subcondylar fracture.

Case Highlights:
1) One of the most common lower jaw fractures is in the subcondylar region right below/at the temporormandibular joint.
2) In a displaced subcondylar fracture where the condyle is out of the joint space, mouth opening is restricted and surgical intervention is required.
3) Open reduction and internal fixation of subcondylar fractures can be done through a preauricular approach if the fracture is high on the neck.
Dr. Barry Eppley
Indianapolis, Indiana