Background: There are a handful of materials that have been historically used for facial implants. While solid silicone is the original and still most commonly used facial implant material even today, other materials have played a more limited but persistent role. The most weak known of these is porous polyethylene, better recognized as Medpor. It is differentiated by its propensity to allow tissue ingrowth, an appealing property to some surgeons and patients alike.
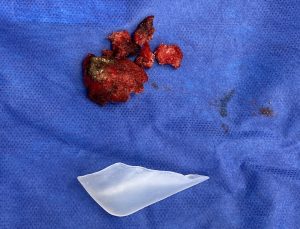
The value of tissue ingrowth into a facial implant material seems to be an intuitive favorable feature… until it is becomes necessary to remove it. Then such tissue ingrowth becomes problematic as the tissue trauma to remove it is far greater than when it was put in. This tenacious tissue ingrowth has many surgeons saying that Medpor can’t be removed or are so challenging and time consuming to do so that they will not do it. The latter may be true but the former is not. Medpor facial implants can be removed but, by silicone facial implant standards, it is far more difficult and requires numerous learned techniques to do so.
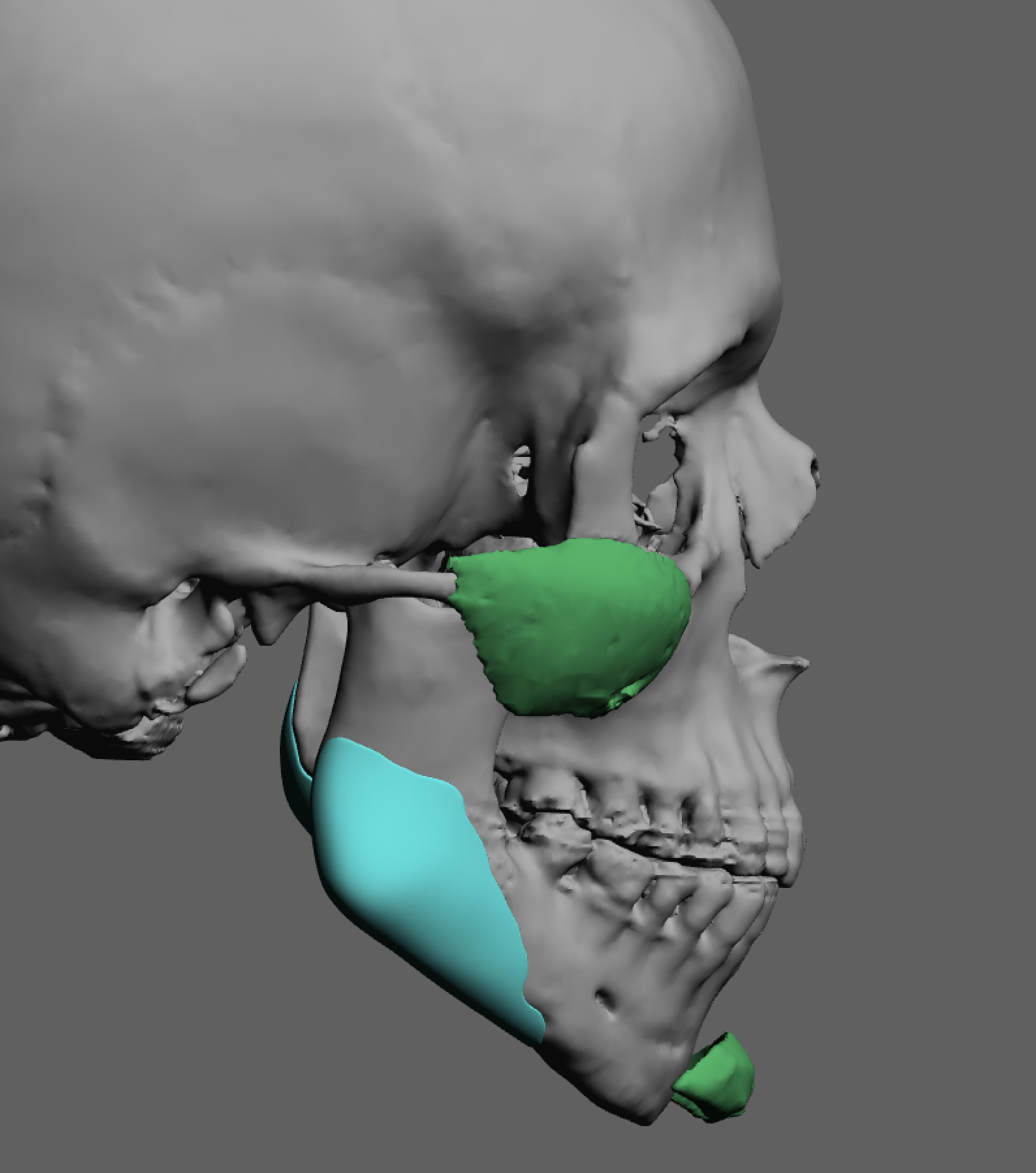
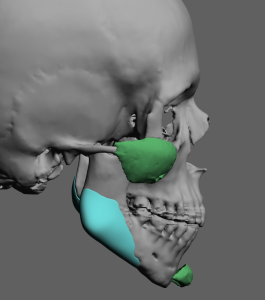
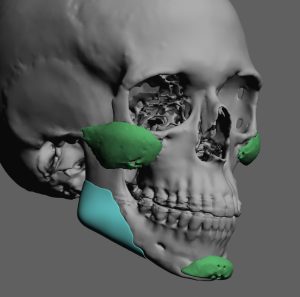
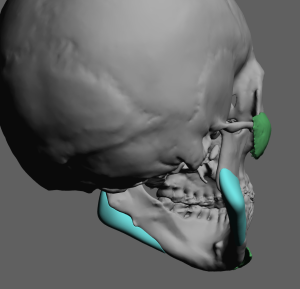
One other property of Medpor implants is that they are not generally visible on 3D CT scans. The tissue ingrowth changes their radiographic appearance to more like soft tissue and not a solid implant material. This poses challenges when trying to evaluate their position on the bone when postoperative implant adjustments are desired/needed or when custom implant replacements are being done. They do appear in regular 2D CT scans but this is really not very helpful as a 3D understanding of their shape and bony position is most desired.
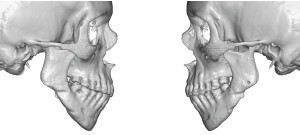
In creating custom jaw angle implants the shape of the bone was used for their design since the existing implants could not be seen. As also seen on the 3D images she had prior implant surgery of the cheeks and chin.

Having taken out hundreds of Medpor facial implants I fail to understand why they continue to be placed. Tissue ingrowth is great…as long as there is never a need to have to adjust, remove or replace the implant. But the reality is that 1/3 of all facial implant patients, whether it is with standard or custom implants, go onto one day to do just that. This case study illustrates that very point even it is 25 years later.
Case Highlights:
1) Medpor jaw angles implants pose challenges for removal with potential injury to various neurovascular structures.
2) Because Medpor implants can not be seen by 3D CT scans, designing new implants around them must use the bony anatomy only.
3) Custom jaw angle implants are the most assured method for the high jaw angle patient where significant vertical lengthening is needed.
Dr. Barry Eppley
Indianapolis, Indiana