Background: The chin is a unique facial structure being a solitary projection that is enveloped by a tight soft tissue chin pad. The chin pad is composed of periosteum, muscle, fat and skin that is adherent around the bone. Like all structural manipulations anywhere on the face how the soft tissue drapes over it does impact the aesthetic outcome. In the chin this soft tissue adaptation is never a problem in augmentation surgery (bony genioplasty and implants) because the soft tissue is expanded and postoperative laxity of it is not a concern.
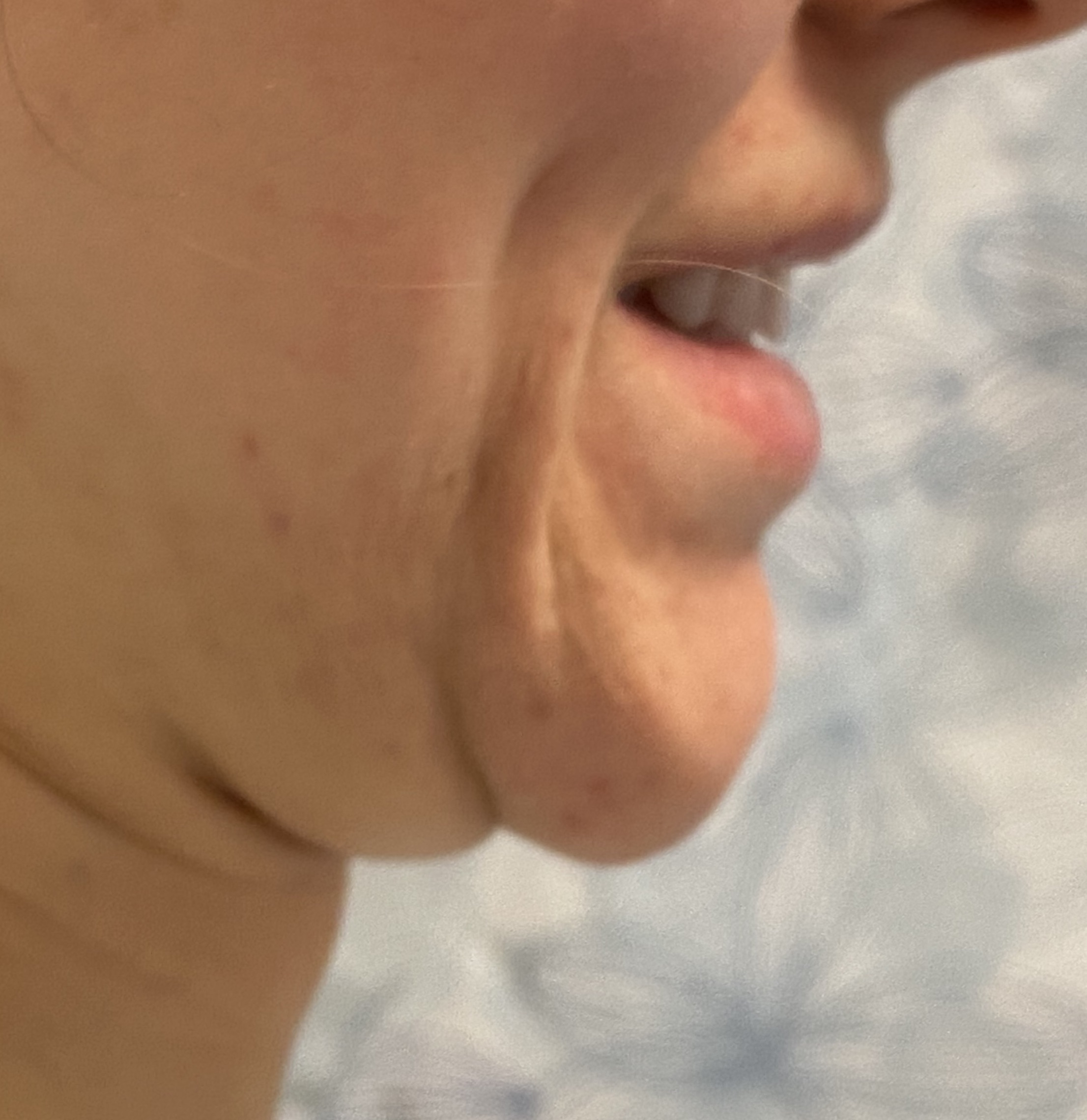
In chin reductions, however, the adaptation of the soft tissue chin pad to a reduced structural support is another matter. This is most manifest in intraoral bony chin reductions by shaving/burring in which the overlying adherent soft tissues have been elevated off of the bone. With less bony support a relative soft tissue excess results which any surgeons assume will merely contract back down and the bone-soft tissue ratio restored. But this is a misconception and some soft tissue laxity will always occur. Whether this newly created soft tissue chin pad excess/laxity is a concern depends on its significance as well as the patient’s perception of it.
Should soft tissue chin pad excess/laxity occur and is a perceived concern the question becomes how to best manage it. It is appealing to try and resuspend the soft tissues intraorally but soft tissue excesses are not usually resolved by lifting. Like soft tissue excesses anywhere on the body excision is the definitive treatment.




Case Highlights:
1) intraoral chin and jaw bony reduction require soft tissue stripping from the bone and its results partially depend on soft tissue contraction…which may not reliably occur particularly of the soft tissue chin pad.
2) Excessive soft tissue chin pad may develop after intraoral bony chin reduction which is most manifest when smiling.
3) Tightening of the lax soft tissue chin pad can only reliably be done from an external submental approach which is ideally placed in a skin crease if it exists.
Dr. Barry Eppley
World Renowned Plastic Surgeon