But today’s 3D CT scans and the design of custom facial implants provides new insights into the biologic behavior of what occurs around all facial implants whether they be custom made or are of standard styles and sizes. And this contemporary 3D CT scan evidence provides a better biologic explanation of what the nature of the bone reaction is to an implanted synthetic material particularly when they are placed on external bone surfaces such as the face and skull.
The starting point of this discussion dates back to some anatomic observations in the early days of craniofacial surgery when onlay bone grafts to the skull and face were commonly used and were an innovative native approach to craniofacial reconstruction. It was noted that they universally underwent a lot of bone remodeling and partial resorption. They lost shape and seemed to have partially ‘melted’ into the underlying and surrounding bone surfaces. Thus was the born the concept of the Biologic Anatomic Boundary. This means that the enveloping soft tissues on any part of the craniofacial skeleton has a certain thickness and tension on the underlying bone for which the bone has developed a certain thickness and shape to withstand. But when the overlying soft tissue envelope is expanded, whether by a bone graft or an implant, it pushes back against it. If a bone graft is \used as the augmentation method the graft will respond to the pressure by modifying its shape until the pressure is relieved, restoring the natural balance between the soft tissue and the underlying bone on which it rests. This, amongst other reasons, is why such onlay one grafts will have an altered shape later.
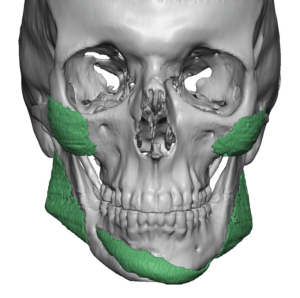
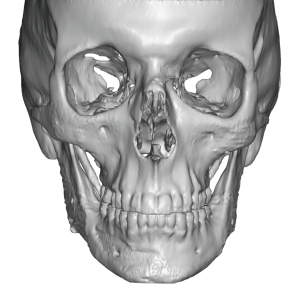
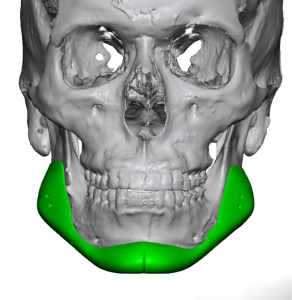
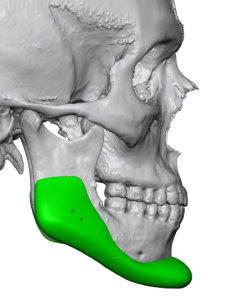
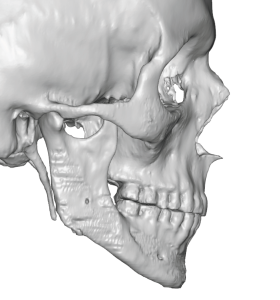
But when it is an implant that is the augmentation method, the implant itself can not change as it is chemically inert. To relieve the pressure of the expanded soft tissues the bone underneath the implant responds to do so. This results in some settling of the implant into the bone as a pressure relief adaptation which results in an impression or imprint of the implant’s shape on the bone which is clearly seen in a 3D CT scan. This process stops when the implant pressure on the bone is relieved. Thus implant bone imprinting is a natural biologic reaction to ‘violation’ of an anatomic boundary which is both self-limiting and of no adverse clinical significance.

Further support of the biologic adaptation to the change in the boundaries of the implantation site is that such bone imprinting occurs regardless of the synthetic material used. Whether it is solid silicone, Medpor (porous polyethylene), PEEK or even titanium such bone imprinting occurs. I have seen it on 3D CT scan with all facial implant materials. The chemical composition of an implant is irrelevant as the basic principle of intrusion into an established soft tissue-bone zone remains the same.

In summary it is time to put aside the historic concept of facial implant ‘bone erosion’ to rest, which implies an inflammatory reaction to the implant that will not cease unless the source is removed. The more contemporary biologic explanation which is clearly shown in 3D facial CT scans, when the existing implants are digitally removed, is a natural self-limiting reaction to an implant placed between the bone and its enveloping soft tissue envelope. The body must relief this infringement on its biologic boundary and does so in the only way it can…modifying the surrounding tissues in response. Because it can be seen in imaging the changes in the surface of the bone can most clearly be seen. Changes in the enveloping soft tissues likely also occur but are currently harder to identify.
Dr. Barry Eppley
World-Renowned Plastic Surgeon