Background: Testicle implants from an aesthetic standpoint have some similarities to breast implants. The end goal is to have an implant in a surrounding sack of skin that is soft, supple and moves without restriction or pain. While the implant type is quite different, a testicle implant is solid silicone while a breast implant is silicone gel in a bag, the success of the concept depends on a surrounding envelope of scar that is thin and pliable. If the surrounding capsule get active and thick it can result in a non-soft implant feel that may even be painful. This is well known in breast implants as capsular contracture. Well it has never been properly identified in testicle implants the same adverse capsular reaction can occur.
I have seen capsular contracture in testicle implants numerous times and is associated with recurrent implant replacements, inadequate pocket dissection and a high superior incisional approach. It may even have a greater occurrence in testicle implants because of a common technique that many Urologists use in placing the implant. They almost always place a permanent suture to hold it in place. In essence they are fixing it into position which is directly contrary to how the natural testicle freely moves. While it is true that the natural testicle is attached to a cord there is no reason that an implant needs an attachment to the scrotum. Such suture fixation prohibits free implant motion which can encourage excessive scar capsule formation and make it feel hard. I have had many patients complain about the suture in that they can both feel it as well as it being uncomfortable. The treatment of such testicle implant capsular contracture is a total capsulectomy with removal of the suture.
The use of the wraparound implant in testicular enhancement has its greatest value when the natural testicles are of normal size. Well this concept is very appealing it has a not insignificant complication rate postoperative separation of the implant sliding off of the testicle. (implant disengagement) As a result this is has tempered its use despite the appeal of the concept. In searching for ways to lessen this risk one approach has been to match the size of the inner chamber of the implant to that of the patients natural testicle with a preoperative ultrasound. This theoretically should lower the risk of that problem as it is easy to see that if the inner chamber is larger than the natural testicle how it would easily slide out. Similarly it is also easy to see that if the natural testicle is larger than the inner chamber (essentially stuffing it into the implant) it could easily be squeezed out after surgery.




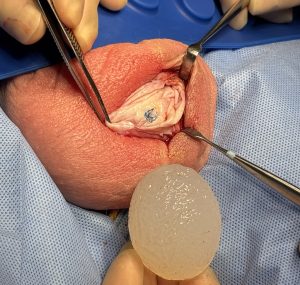
In this unique case two different styles of custom testicle implants were used. On the left side where a solid implant was used as a replacement a very significant capsular contracture was seen and treated by a capsulectomy. Coming from an inferior approach to the capsule helped create a larger and anexpanded pocket down into the lower end of the scrotum. This is one of the advantages the low midline scrotal incisional approach. On the opposite right side given the size of the natural testicle and to keep pace with the larger implant on the left side, the only option was a wraparound style implant. Hopefully matching the size of the natural testicle to the inner chamber design of the implant will help lower the risk of postoperative separation.
Key Points:
1) Testicle implants like breast implants can develop capsular contracture.
2) In treating testicle implant capsular contracture a total capsulectomy with suture removal is needed.
3) T ballou what are you doingo decrease the risk of postoperative separation in wraparound testicle implants the size of the internal chamber should match that of the size of the patients natural testicle.
Dr. Barry Eppley
World-Renowned Plastic Surgeon