The most common potential adverse affect relating to facial implants is the concern about bone erosion. While this is certainly not the most common complication from facial implants it is certainly one that is widely spoken about albeit biologically incorrect. The term erosion goes back over 50 years from looking at some chin implants in lateral cephalometric x-rays. It could be seen that in some patients that the implant has settled into the bone. This was particularly evident in implants that were positioned high on the chin bone where the outer cortex is thinner. (and under more pressure from the origin of the mentalis muscle.) In very rare cases the tooth roots may be at risk.
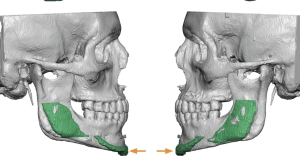
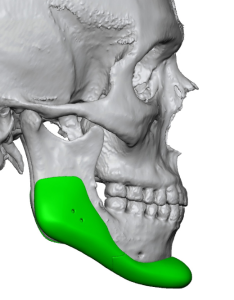
As a result of these historic x-ray findings facial implants, particularly chin implants, have become associated with causing long term bone loss. But this interpretation of what happens around lower facial implants fails to appreciate the actual biology of how the body responds to the interposition of an implant into its tissue planes. Since a plain x ray served as the basis for the erosion supposition more contemporary 3D CT scan imaging shows a different and more complete understanding of the biologic response to the placement of an implant on the mandible.

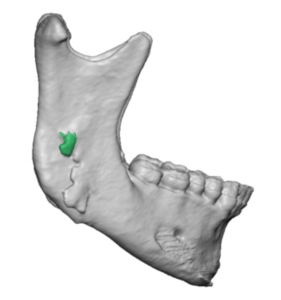
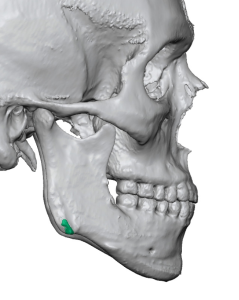
What does these 3D CT scan findings tell us about the biology of facial implants? First and foremost it is clear that an inflammatory reaction to them is not what is occurring. The clear and sharply defined imprint borders of the implant make that evident. If it was an inflammatory reaction (erosion) the pattern of the implant on the bone would be irregular and indistinct and have an almost ‘moth-eaten’ appearance. Secondly an inflammatory reaction would not result in any evidence of bony overgrowths. Inflammatory cells are destructive not regenerative. Bony overgrowths are a sign of a healing response, trying to heal over the implant.
The key concept to grasp in any form of aesthetic augmentation, and craniofacial augmentation in particular because the bony response can be more clearly seen, is that of the violation of anatomic boundaries. The tissues at any implantation have formed to support what has developed around them. When you introduce an implant, which exerts its augmentation effect by pressure and can not physically change its shape, the tissues around it must adapt to the pressure that has now been exerted onto them. A natural pressure relief results which is seen by some implant settling into the bone which occurs in varying degrees. Once this pressure relief has occurred it stops resulting in a response to the implant that is not progressive. (self-limiting)
Dr. Barry Eppley
World-Renowned Plastic Surgeon