Introduction
Jaw angle implant asymmetry, whether resulting from standard implants or a custom jawline implant, is not uncommon. Several factors contribute to this, including limited visibility through the intraoral incision used for placement, incomplete elevation of the masseteric muscle, or unrecognized differences in bony jaw angle morphology.
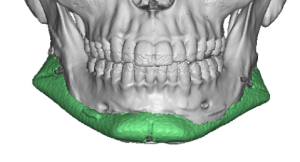
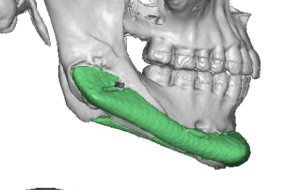
Once full healing has occurred (typically three months or more postoperatively) and the final contour is evident, a 3D CT scan should be obtained to assess implant positioning precisely. Although some implant materials are less radiographically visible, those that are will clearly show the cause of asymmetry. In most cases, the discrepancy arises from an implant positioned too high rather than too low.
The usual corrective approach is through the intraoral incision, the same route used during the original placement. This method is effective in most cases since identifying where the implant should not be helps determine where it should be. However, some patients may prefer to avoid another intraoral procedure due to the associated recovery, infection risk, or prior healing issues.
An alternative external (transcutaneous) approach offers a more direct route with a lower risk of infection and a potentially more precise means of repositioning the implant.
Case Study
To ensure accurate repositioning and avoid re-entering the mouth, a direct external incision was selected.


Discussion
The direct transcutaneous approach to the jaw angle region has been described in reconstructive surgery but, to my knowledge, not previously in aesthetic implant revision. It has proven to be a safe and effective option in select cases. The resulting fine-line scar is typically well tolerated in male patients; however, scar acceptability in female patients remains a concern due to cosmetic visibility.
A key consideration is the proximity of the marginal mandibular branch of the facial nerve, which runs below the jaw angle. When the head is turned during surgery, this nerve can be drawn closer to the operative field. To avoid injury, the incision should be made directly over the jaw angle, dissection should be blunt and anterior, and electrocautery should be avoided.
This approach should be viewed as a tunnel technique rather than one that allows wide exposure. Despite its limited visibility, it provides sufficient access for implant repositioning and secure screw fixation.
Placement and revision of jaw angle and custom jawline implants are inherently challenging due to the complex anatomy and posterior location of the mandible. Surgeons performing such procedures must be proficient in both intraoral and external revision techniques to address potential complications effectively.
Key Points
-
Jaw angle implant asymmetry is most commonly due to a high implant position.
-
A 3D CT scan is essential to accurately diagnose implant positioning.
-
The transcutaneous approach offers a safe, direct alternative for implant repositioning.
-
Careful technique is required to avoid injury to the marginal mandibular nerve.
-
Proper patient selection is critical, as scar visibility may limit use in female patients.