Introduction
Reduction osteotomies of the clavicle for shoulder reshaping (shoulder narrowing or “desquaring”) follow the same core biological principles as fracture healing, but with nuances related to clavicular anatomy, vascularity, and rigid fixation. Healing typically progresses through four well-established phases:
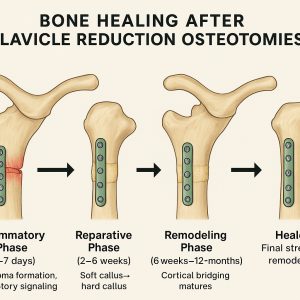
Inflammatory Phase (0–7 days)
- Hematoma formation and initiation of inflammatory signaling
- Recruitment of osteoclasts and osteoblasts
- Rigid fixation is essential to limit micromotion and support early healing
Reparative Phase (2–6 weeks)
- Transition from soft callus to hard callus
- Rigid plating often promotes primary (intramembranous) bone healing with little visible callus
- Early radiographic consolidation is often observed by 4–6 weeks
Remodeling Phase (6 weeks – 12+ months)
- Cortical bridging matures and osteons reorganize
- Mechanical strength returns substantially by 3–6 months and continues to improve for up to a year
2. Expected Healing Timeline
|
Timeframe |
Typical Findings |
|
2 weeks |
Early stability; pain reduction; soft callus or early primary bone union begins |
|
6 weeks |
Radiographic signs of union commonly present; resumption of light daily activities |
|
2 months |
Solid union in most cases; heavier use allowed depending on symptoms and fixation |
|
3–4 months |
Advanced remodeling; return to high-impact or contact sports if union is robust |
Healing outcomes for clavicle reduction osteotomies are excellent. Contributing factors include patient health, nonsmoking status, precise surgical cuts, excellent bone apposition, and dual-plane rigid fixation.
- Typical union rate: >99%
- Nonunion rate: <1% with stable modern plating
Radiographs often cannot clearly show the osteotomy line due to hardware density and the narrow end-to-end interface. The most definitive assessment of union typically occurs during later hardware removal when indicated. Hardware prominence may develop in patients with minimal soft-tissue coverage and is most often addressed 9–12 months post-operatively, once consolidation is complete.
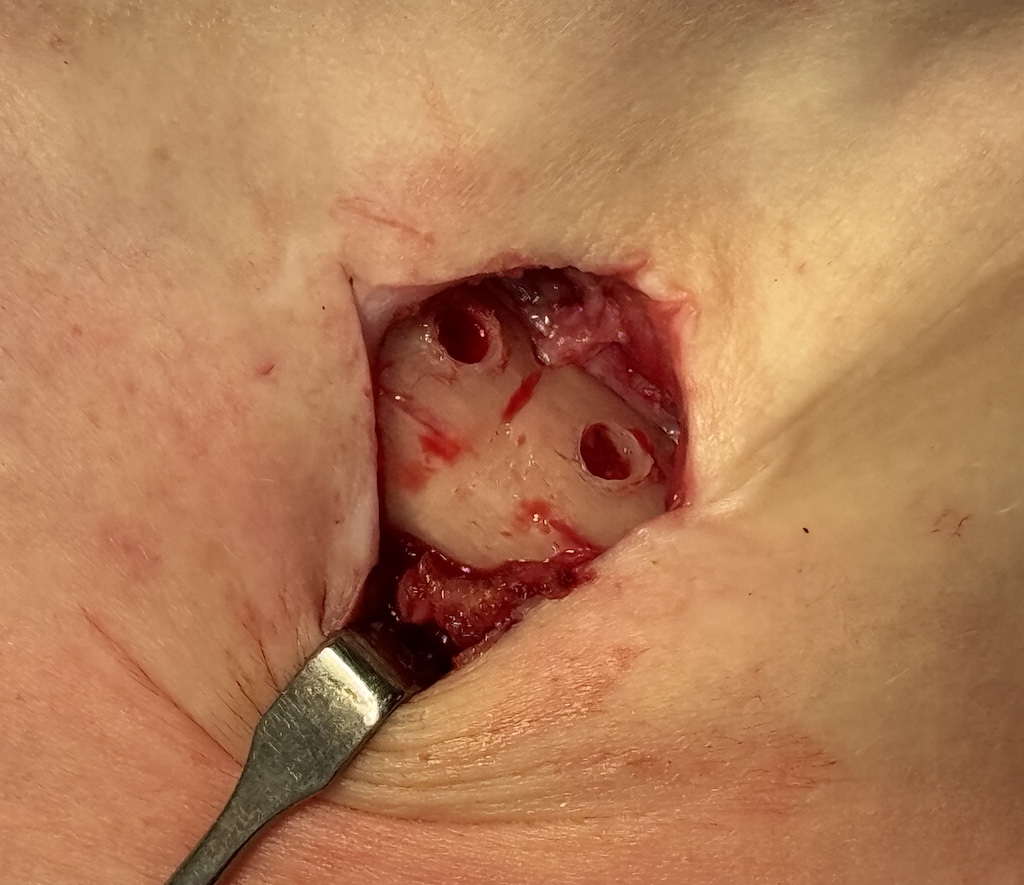
Case Study




- Typical bony ingrowth into the screw threads—especially within the superior 3.5 mm plate—was observed.
- Examination of the osteotomy sites showed a barely perceptible line with complete, solid bridging bone, consistent with primary bone healing.
Discussion
Clavicle shortening osteotomies generally heal more predictably and quickly than traumatic clavicle fractures due to:
- Controlled osteotomy cuts with sharp, uniform edges
- Minimal soft-tissue disruption and preserved blood supply
- Excellent end-to-end bone contact
- Rigid dual-plate fixation enabling primary, callus-free bone healing
As a result, osteotomies often heal 1–2 months faster than comparable fractures.
Despite the excellent visual and tactile evidence of union at one year, the healed osteotomy site may still be slightly weaker than the native bone initially due to:
- Stress shielding from hardware, which reduces functional loading and thus bone density during early healing
- Slight mismatch in bone diameter where the resected ends meet, leading to a marginally reduced cross-sectional area
After hardware removal, normal functional loading encourages the osteotomy region to regain near-normal density and strength. Clinically, this supports the recommendation to avoid heavy lifting or strenuous shoulder activity for several months following device removal.
Key Points
- A small percentage of shoulder-reduction patients will experience hardware prominence requiring secondary removal.
- Hardware removal provides the only direct opportunity to visually assess osteotomy healing.
- Due to stress shielding and the clavicle’s narrow diameter, patients should avoid strenuous upper-body activity for 1–2 months following hardware removal.
Dr. Barry Eppley
World-Renowned Plastic Surgeon