Introduction
Total temporomandibular joint (TMJ) replacement is a surgical procedure in which a damaged jaw joint is replaced with a biocompatible prosthesis to relieve pain and restore function when conservative treatments have failed. It is most commonly indicated for severe degenerative joint disease, including osteoarthritis and rheumatoid arthritis, as well as advanced joint destruction, deformity, or resorption.
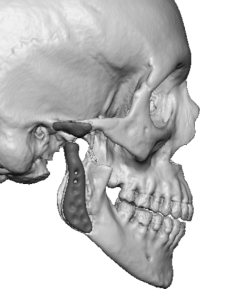
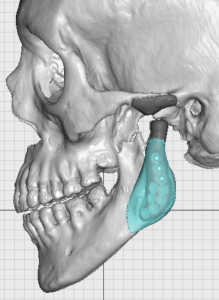
Modern TMJ replacements are custom-made prostheses designed from the patient’s three-dimensional CT scans. This approach allows for precise adaptation to the patient’s anatomy, improved jaw alignment, and more predictable long-term outcomes. The prosthesis consists of two components: a mandibular component that replaces the condyle and is fabricated from a titanium alloy, and a fossa component that replaces the socket and is made from ultra-high-molecular-weight polyethylene (UHMWPE).
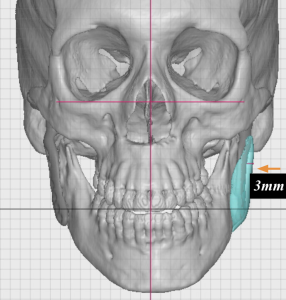
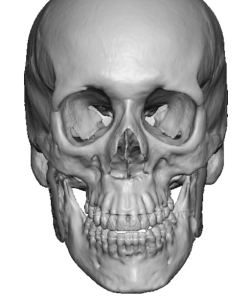
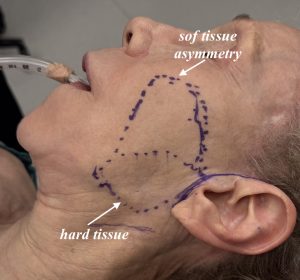
Although TMJ replacement reliably improves joint function, it does not address pre-existing bony jaw angle asymmetry. In addition, surgical trauma can contribute to postoperative soft-tissue thinning or volume loss, which may further accentuate facial asymmetry. Correction of such asymmetry may therefore require additional custom bony implants and/or soft-tissue augmentation for optimal aesthetic improvement.
Case Study




Discussion
Facial asymmetry commonly consists of both hard- and soft-tissue components, each requiring a different corrective strategy, even when addressed during the same operation. The hard-tissue component can be accurately quantified using three-dimensional CT imaging. The presence of hardware in the jaw angle region does not preclude the design or placement of custom implants, and a TMJ prosthesis does not pose additional challenges in this regard.
The soft-tissue component of facial asymmetry is determined primarily by clinical assessment and estimation of the volume deficit. Although fat grafting remains the most common and versatile method of soft-tissue augmentation, retention rates in thin, older patients are often poor. In such cases, dermal grafts placed through facelift-type incisions and flaps provide a more reliable and sustained, albeit modest, augmentation effect.
Key Points
- Total TMJ replacement provides significant functional improvement but does not correct existing facial asymmetry and may accentuate it.
- Custom jaw angle implants can be designed to overlay the ramus component of a TMJ prosthesis to correct structural asymmetry.
- Soft-tissue facial asymmetry can be effectively augmented with allogeneic dermal grafts when fat grafting has failed.
- By combining a custom jaw implant with soft-tissue support, facial asymmetry after TMJ replacement can be safely and predictably improved.
Barry Eppley, MD, DMD
World-Renowned Plastic Surgeon