Introduction
Scalp roll excision is a minor surgical procedure used to remove a redundant fold or “roll” of skin at the back of the scalp or upper neck—most commonly in the occipital/posterior neck area.
What it treats
- Prominent horizontal scalp or neck rolls
- Skin redundancy after weight loss
- Excess tissue following prior neck or scalp surgery
- Congenital or age-related skin laxity in the occipital region
How the procedure is done
- Marking: The skin roll is marked with the patient upright so the fold is clearly defined.
- Excision: An elliptical strip of skin and subcutaneous tissue is removed, usually oriented horizontally within a natural crease.
- Laterally avoid injury to the greater occipital nerve.
- Closure: The wound is closed in layers to minimize tension and improve scar quality.
- Setting: Performed under general anesthesia in the prone intraoperative position.
Scar location
- The scar is placed within or just above the natural posterior neck crease, so it is usually well hidden by hair or natural folds.
Recovery
- Outpatient procedure
- Mild swelling and tightness for 1–2 weeks
- Absorbable sutures uses, no need for removal.
- Return to normal activities in a few days, avoiding heavy strain initially
Risks & considerations
- Scar widening or visibility (uncommon with proper placement)
- Temporary numbness or tightness
- Asymmetry or recurrence if skin laxity progresses
- Careful roll excision marking is needed to avoid incomplete roll removal.
Case Study





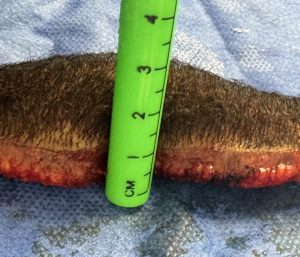
Discussion
In scalp roll excision, the safe amount of scalp/skin that can be removed is governed by tension, vascularity, and closure quality, not by a fixed measurement.
Practical safe ranges (clinical guidelines)
- Width (anterior–posterior pinch):
- 1.5–2.5 cm is routinely safe in most patients
- Up to ~3 cm can be removed only if the scalp roll pinches easily and closes without tension
- 3 cm markedly increases risk of wound tension, scar widening, and discomfort
- Length (medial–lateral):
- Can extend across the entire visible roll (often 8–15 cm or more)
- Length is usually not the limiting factor as long as closure tension is controlled
Key intraoperative safety principles
- Pinch test is critical
- If the roll closes comfortably with finger approximation while the head is neutral, it is usually safe.
- If closure requires force or neck flexion ? over-resection.
- Preserve subdermal vascularity
-
- Can be done to the periosteum centrally but stay superficial to the deep fascia laterally to avoid greater occipital nerve injury.
- Tension-free layered closure
-
- Deep dermal sutures must carry the load.
- Skin sutures should be passive, not load-bearing.
Patient-specific modifiers
- Significant lscalp axity: can tolerate slightly wider excisions
- Thick stiff fibrotic scalp: be conservative
- Massive weight loss patients: often tolerate wider excisions
Key Points
1) Double roll scalp surgery requires one full scalp roll excision and part of the other roll.
2) Avoid deep roll excision laterally to avoid greater occipital neurovascular bundle.
3) Realistic expectations about a linear scar in exchange for back of head contour improvement.






