Custom infraorbital–malar implants are one of the most powerful (and under-used) solutions for true undereye hollowing, especially when the problem is skeletal deficiency, not just soft-tissue fat loss (e.g., after lower blepharoplasty)
Undereye hollowing is often caused by:
- Infraorbital rim deficiency
- Negative vector midface
- Low malar projection with deep tear trough
- Thin lower-lid soft tissue draping over bone
Fillers and fat can camouflage this temporarily, but they don’t correct the bony foundation. Custom implants do.
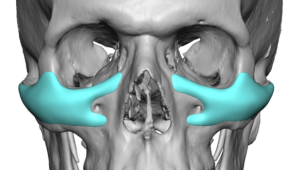
What “custom infraorbital–malar” (IOM) really means
These are patient-specific implants designed from CT data to:
- Restore infraorbital rim projection
- Smooth the lid–cheek junction
- Add malar support without lateral overprojection
- Eliminate the tear trough by lifting the platform, not filling the groove
They are not just malar shells or rim strips—they are continuous anatomical units that function to expand the bony contours in a smooth fashion.
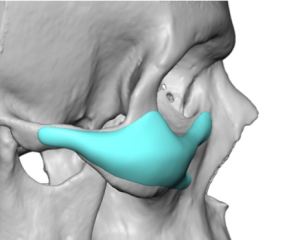
IOM Implant Key Design Elements
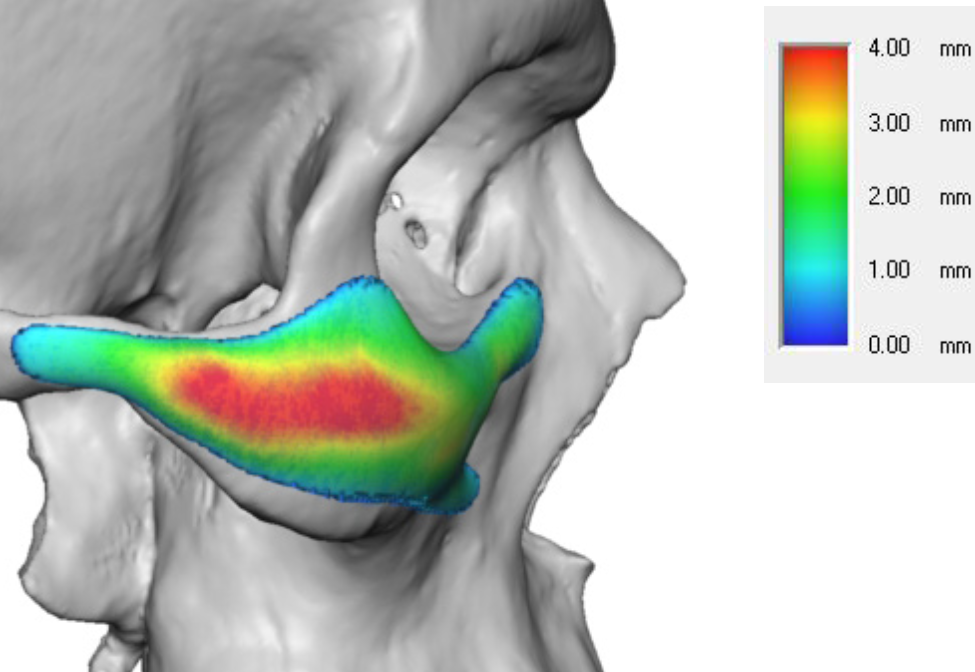
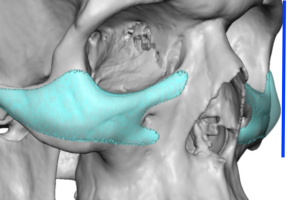
1. Infraorbital segment
- Precise rim augmentation that saddles the rim adding both vertical and horizontal increases (usually 2–4 mm)
- Extends from near nasal bone medially to around the lateral orbital rim
- Smooth inferior, medial and lateral transitions to avoid step-offs (feather edging)
- Avoids encroachment on infraorbital foramen
2. Malar segment
- How significant the malar component is depends on whether the primary focus of the IOM implant is infraorbital, malar or equally shared.
- Could be anterior or lateral based-focused projection based on patients aesthetic needs and gender
- The malar projection in the oblique view should have an even double Ogee convexity curves.
3. Tear trough elimination
- Comes from the subperiosteal release of the arcus marginalia and the fill volume provided by the rim augmentation
- Creates a smoother lid–cheek continuum
Materials
Most commonly:
- Solid silicone (Silastic) – preferred by many for:
- Ease of insertion/removal
- Smooth edges
- Minimal inflammatory response
- PEEK – does not have feathered edges of the rim is vertically augmented, harder to revise, not available in the U.S.
- Porous polyethylene (Medpor) – the least favored due to bulky designs, lack of fine feathered edges and removal challenges.
For undereye aesthetics, smooth silicone often gives the best blend and lowest complication profile.
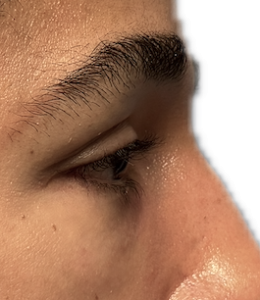
Case Study
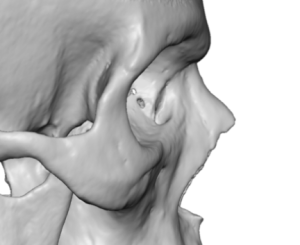
backward malar inclination in the side view.
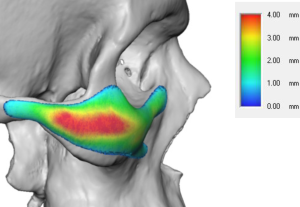
Implant thicknesses must consider how much vertical and horizontal rim augmentation is desired as well as the amounted line of malar projection..

Discussion
The ideal candidates for IOM implants are:
- Persistent tear trough despite filler/fat
- Hollowing that worsens with smiling
- Lower lid retraction/ inferior scleral show
- Negative vector anatomy
- Prior unsatisfactory filler or fat injection history
They are not for patients that have:
- Isolated thin-skin hollowing without skeletal deficiency
- Severe lower lid laxity without lid support correction
- Patients seeking temporary change
Common IOM implant design pitfalls (avoidable)
- Over-projecting the malar portion ? unmmnatural cheek protrusion
- Sharp implant edges ? visible transitions
- Failure to saddle the infraorbital rim
- Too low malar projection
- Inadequate implant footprint for implant thickness
Bottom line
For true undereye hollowing driven by bone deficiency, custom infraorbital–malar implants are:
- More anatomically correct
- More predictable
- More durable than fillers or fat—and often safer long-term for the lower lid.
- Should be first line treatment for negative orbital vector anatomy
- An important design concept in the sensitive orbital-cheek area is to understand that 1 or 2mms in implant projection can make a big difference in its effect.
Dr. Barry Eppley
World-Renowed Plastic Surgeon