Indications
- Patients desiring central buttock projection with limited donor fat
- Lean or athletic patients where subcutaneous coverage is inadequate
- Revision of subfascial/subcutaneous implants with visibility or palpability
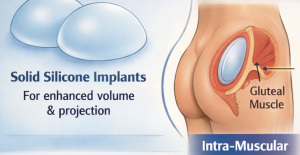
Relevant Anatomy
Gluteus maximus: thick, quadrilateral muscle; fibers run inferolaterally
- Safe zone: upper and central muscle belly
- Avoid:
- Superior gluteal neurovascular bundle (deep, superior)
- Inferior gluteal vessels (deep, inferior)
- Sciatic nerve (deep, inferomedial)
The intramuscular pocket is typically 2–3 cm deep, not a full muscle split.
Surgical Technique
1. Positioning & Marking
Prone position
- Mark:
- Midline intergluteal crease or bilateral paramedian incisions. Paramedian incisions are indicated when the interglutealk area is very ‘bony’ with little subcutaneous fat tissue.
- Lateral buttock borders
- Planned implant footprint (usually centered over maximal projection point)
2. Incision
- 5–7 cm incision in the intergluteal crease or 5cm paramedian incisions
- Dissection carried down to the gluteal fascia, preserving dermal blood supply. The fascia is closer from the paramedian incisions.
3. Muscle Entry
- The gluteus maximus muscle fibers is identified below the fasci.
- Entry point typically 3–4 cm lateral to midline
- Split muscle fibers bluntly after opening the fascia
4. Intramuscular Pocket Creation (Key Step)
- Create pocket within the muscle belly
- Dissection plane:
- Approximately half the muscle thickness 2 to 3cm deep
- Blunt finger identifies depth
Pocket dissection
- Moist lap sponges do the direction bluntly
- The goal is to get 3 lap sponges snugly into the pocket. Each lap sponge = 100cc implant volume. The average implant placement is in the 250cc to 400cc range.
5. Hemostasis
- The lap sponge blunt dissection technique paralleling the muscle fibers creates very little bleeding. Occasionally a perforator will be avulsed and is controlled by bipolar cautery under direct vision. If bleeder is deeper, and not in direct vision pack until the vessel constricts on its own.
6. Implant Selection & Insertion
- Solid silicone elastomer implants
- Common shapes:
- Round or oval (surgeon preference)
- Typical sizes:
- 250–400 cc (varies by frame and muscle thickness)
- Irrigation with antibiotic solution
Implant inserted deep into pocket with aid of the funnel insertion device which overcomes the dramatic difference in width between the incision and the implant base diameter.
- The implant will often not completely unfold and the pocket is expanded with a blunt instrument around the implant’s perimeter until it passively lays flat and rests easily underneath the muscle opening near the incision.
7. Closure
Muscle split/fascial closure using 2-0: absorbable interrupted sutures
- Muscle closure should be complete over implant without undue tension over the implant. (The sutures will tear through the muscle fibers if the implant is not resting passively beneath it which means an inadequately created pocket)
Dermal and skin closure in layers
- Drains:
- Surgeon-dependent
- Bilateral closed-suction drains may be used
Postoperative Protocol
- Prone or lateral positioning for 2–3 weeks
- Avoid sitting directly on buttocks early
- Compression garment after initial healing
- Gradual return to activity at 4–6 weeks
Advantages of Intramuscular Placement
- Better implant camouflage
- Lower rates of:
- Palpability
- Edge visibility
- Inferior mplant migration
- Infection
- Seroma
- More natural contour than subfascial
Common Complications & Prevention
|
Complication |
Prevention Pearl |
|
Implant migration |
Tight, symmetric pocket |
|
Seroma |
Drains + limited dead space |
|
Infection |
Strict hemostasis, minimal implant handling |
|
Muscle atrophy |
avoid superficial muscle pocket dissection |
|
Asymmetry |
Pre-op markings + intra-op symmetry checks |
Technical Pearls
- The most common error is dissecting too superficial ? eventually ends up subfascial with muscle atrophy
- Implant must lie passively fully unfolded in the intramuscular pocket with tension free closure of the muscle over it
- Stay central—lateral overdissection increases implant edge show as it pops out from under the muscle
- Revision cases often require new intramuscular pocket underneath existing capsule
The intramuscular pocket has numerous advantages over the more superficial subfascial pocket location in both improved aesthetic outcomes and lower complication rates. How the intramuscular pocket compares to the ‘newer’ complete submuscular pocket location for buttock implants remains to be determined.
Dr. Barry Eppley
World-Renowned Plastic Surgeon




 Gluteus maximus: thick, quadrilateral muscle; fibers run inferolaterally
Gluteus maximus: thick, quadrilateral muscle; fibers run inferolaterally
 Prone position
Prone position Pocket dissection
Pocket dissection

 Implant inserted deep into pocket with aid of the funnel insertion device which overcomes the dramatic difference in width between the incision and the implant base diameter.
Implant inserted deep into pocket with aid of the funnel insertion device which overcomes the dramatic difference in width between the incision and the implant base diameter.
 Muscle split/fascial closure using 2-0: absorbable interrupted sutures
Muscle split/fascial closure using 2-0: absorbable interrupted sutures
 Dermal and skin closure in layers
Dermal and skin closure in layers