The intercostal nerve is a critical structure that must be carefully respected during rib removal or rib contouring surgery. Failure to properly manage this nerve can result in long-term pain complications.
Intercostal Nerve Anatomy

Order (superior ? inferior):
- Vein
- Artery
- Nerve (most inferior and most vulnerable)
The intercostal nerve lies within the costal groove on the undersurface of the rib. It does not separate easily from this groove and therefore requires careful, deliberate dissection. Prior to any rib cutting, the nerve must be dissected free and protected.
Intercostal Nerve Injury
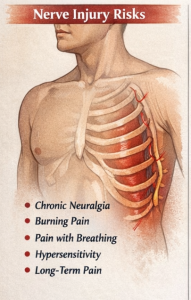
- Chronic intercostal neuralgia
- Burning or stabbing pain
- Pain with breathing, twisting, or coughing
- Hypersensitivity or dysesthesia
- Persistent pain lasting years (sometimes permanent)
This is why rib removal, if not performed carefully, can result in significant and disturbing symptoms despite its aesthetic benefits.
Nerve-Protective Principles in Rib Contouring
A. Subperiosteal Dissection (Critical)
- Dissection must remain directly on bone.
- The periosteum should be elevated andpreserved.
- The nerve remains protected beneath the periosteal layer.
When the periosteum is stripped inferiorly, the nerve becomes exposed. While this may seem counterintuitive, visualization of the nerve is essential. Seeing the nerve as dissection proceeds around it is paramount to ensuring it remains intact. The goal is controlled release—not blind manipulation.
B. Superior-to-Inferior Working Direction
To optimize nerve safety, subperiosteal dissection proceeds from the superior to the inferior rib border.
- Dissection begins along the superior border.
- The surgeon works underneath the rib toward the inferior border.
- At the inferior edge, the neurovascular bundle is carefully elevated from the costal groove.
This connects the superior subperiosteal dissection with controlled release of the neurovascular bundle.
C. Segment Length
The length of rib removed does not determine nerve injury risk. Adequate neurovascular release does.

D. End Smoothing and Beveling
Sharp rib edges can cause chronic irritation.
- Cut ends should be rounded and beveled.
- This reduces the risk of nerve compression and scar-related irritation.
E. Nerve Dissection Principles
- Circumferential rib skeletonization is necessary.
- Subperiosteal circumferential dissection is essential.
- The nerve should be visualized and freed.

F. Ribs 11 and 12: Safer—but Not Risk-Free
Ribs 11 and 12 are generally lower risk because they are:
- More mobile
- Shorter in neurovascular course
- Less involved in respiratory mechanics
However, nerve injury can still occur and may result in:
- Flank pain
- Abdominal wall dysesthesia
Clinical Pearl
Chronic pain after rib removal does not originate from the bone itself. If it occurs, it is the intercostal nerve’s response to how it was managed during surgery.
Potential postoperative nerve complications can be minimized through:
- Circumferential subperiosteal dissection techniques
- Careful elevation of the neurovascular bundle from the inferior costal groove
- Direct visualization and controlled release of the nerve during proximal-to-distal rib dissection
Dr. Barry Eppley
Plastic Surgeon





