There are numerous strategies for structural midfacial augmentation, some of which are less commonly recognized due to their lower frequency of use. One such procedure is central midface projection enhancement, anatomically termed infraorbital–maxillary augmentation.
Infraorbital–maxillary augmentation refers to surgical enhancement of the infraorbital rim and anterior maxilla to improve under-eye support, increase midface projection, and enhance overall facial balance.
Today, this region is most commonly treated with injectable fillers or fat grafting. While these methods can produce improvement, fillers require repeated treatments to maintain results, and fat grafting may lack long-term volume persistence. For patients seeking a more permanent and structurally reliable solution, implant-based augmentation offers a definitive alternative.
Indications
Aesthetic Indications
- Infraorbital hollowing / negative vector midface
- Tear trough deformity not adequately correctable with fillers
- Flat or recessed anterior maxilla
- Poor lower eyelid support
- Aging-related midface retrusion
- Desire for increased midfacial projection
Relevant Anatomy
- Infraorbital rim
- Anterior maxilla (paranasal region)
Infraorbital nerve (V2 branch)
The infraorbital nerve exits approximately 6–10 mm below the infraorbital rim and must be carefully identified and protected during surgery.
Implant-Based Augmentation
Surgical Approach
- Intraoral vestibular incisions
- May be combined with a lower eyelid approach for extended implant designs for assured placement
Implant Material Options
- Silicone
- PEEK
- Porous polyethylene (Medpor)
Advantages
- Precise control of projection
- Immediate structural support
- Reversible
Custom vs. Standard Implants
|
Feature |
Standard Implant |
Custom Implant |
|
Fit |
Generic |
Patient-specific |
|
Symmetry Control |
Limited |
Excellent |
|
Cost |
Lower |
Higher |
|
Ideal For |
Mild augmentation |
Moderate–severe deficiency |
In practical application, custom implants are almost always used for infraorbital–maxillary augmentation, as no true standard implants exist for this specific anatomical region.
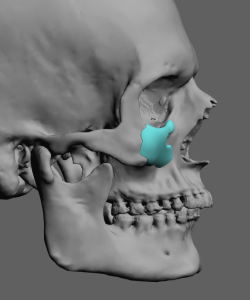
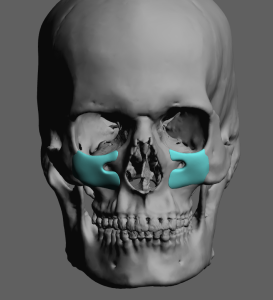
Extended designs may incorporate the paranasal, premaxillary, and malar regions. These broader constructs are often referred to as custom midface mask implants.
Aesthetic Goals
- Improved lower eyelid support
- Reduction of tear trough shadowing
- Smooth transition between eyelid and cheek
- Increased midface convexity
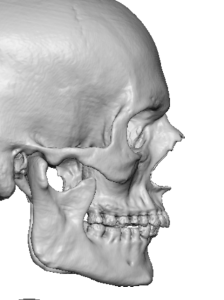
- Improved overall facial harmony (particularly in profile view)
Risks and Complications
- Infraorbital nerve numbness (temporary or permanent)
- Implant malposition
- Infection
- Over- or under-projection
Recovery
- Swelling: Most significant during the first 1–2 weeks; residual swelling may persist 2–4 weeks
- Final contour assessment: Approximately 2–3 months
- Bruising: Variable
- Numbness: Common initially; typically temporary
Case Example
This male patient previously underwent fat injections to the infraorbital and adjacent midface region to treat tear trough deformity and deficient projection. Although early results were satisfactory, the augmentation was completely resorbed within six weeks.
Rather than repeat fat grafting, he elected to proceed with permanent implant augmentation.

Design Principles for Custom Infraorbital–Maxillary Implants
1. Define the Deformity First — Not the Implant
Implant design must follow the skeletal deficiency pattern rather than aesthetic trends.
Evaluate in Three Planes:
A. Sagittal (Projection)
- Negative vector midface
- Infraorbital rim retrusion
- Paranasal depression
- Flat anterior maxilla
B. Vertical
- Inferior orbital rim deficiency
- Short midface
- Excess scleral show due to skeletal support loss
C. Transverse
- Narrow anterior maxilla
- Asymmetry
- Unilateral hypoplasia
Key Principle:
Projection should restore skeletal harmony — not create anterior bulk or fullness.
2. Zonal Implant Design Strategy
Divide the implant into functional zones:
Zone 1: Infraorbital Rim
- Provides lower eyelid support
- Must follow the natural orbital curvature
- Avoid overprojection to prevent an unnatural lid–cheek junction
Zone 2: Medial Infraorbital / Tear Trough Support
- Smooth convex transition
- No sharp edges beneath thin skin
- Blended inferiorly to prevent step-offs
Zone 3: Paranasal (Anterior Maxilla)
- Corrects pyriform and subalar depression
- Critical for profile improvement
- Supports the nasolabial angle
Zone 4 (Optional): Malar Transition Extension
- Smooth lateral blending into the zygoma
- Prevents visible implant demarcation
Design Rule:
The implant should function as a continuous topographic augmentation — not a focal bump on bone.
3. Thickness Distribution Principles
Maximum Projection Zone
Typically located:
- Just inferior to the infraorbital rim
- Or within the paranasal depression
Feathered Edges
All borders must taper to 0 mm, especially:
- Inferior border
- Lateral transition
- Medial orbital rim
Avoid the “Shelf Effect”
Overbuilding directly beneath the orbital rim may create:
- Visible ridging
- Lower eyelid stiffness
- An artificial appearance
Instead, create a gradual anterior sweep.
4. Relationship to the Lower Eyelid
The implant should:
- Improve eyelid support
- Potentially reduce negative vector (secondary effect)
- Decrease tear trough shadow
5. Infraorbital Nerve Management
- Design nerve relief directly into the implant
- Ensure the implant sits slightly inferior to the nerve exit
- Avoid compressive geometry
6. Asymmetry Correction
Custom implants allow:
- Differential thickness
- Volume redistribution
- Vertical rim leveling
7. Projection Guidelines (General Aesthetic Ranges)
(Case dependent — not rigid values)
Infraorbital rim: 2–3 mm
Maxilla: 4–6 mm
Projection beyond 5–6 mm requires careful transition design to avoid unnatural fullness.
8. Soft Tissue Considerations
Even optimal skeletal design will fail if soft tissue dynamics are ignored.
Evaluate:
- Skin thickness
- Suborbicularis fat
- Malar fat pad position
- Lower eyelid tone
Thin-skinned patients require:
- Softer transitions
- Lower projection thresholds
Aesthetic Philosophy
The goals of infraorbital–maxillary augmentation are:
- Structural support
- Natural light reflection
- Smooth lid–cheek transition
- Improved facial convexity
- Elimination of dependency on injectable augmentation
The procedure should not produce:
- An artificial “filled” appearance
- Excess midface bulk
- Visible implant contours
The infraorbital-maxillary implant is a vertical midface augmentation which differs it from the custom infraorbital-malar implant which is a horizontal midface augmentation. Both carry the acronym IOM but have different midface implant designs and augmentation effects.
Dr. Barry Eppley
Plastic Surgeon




 Infraorbital nerve (V2 branch)
Infraorbital nerve (V2 branch)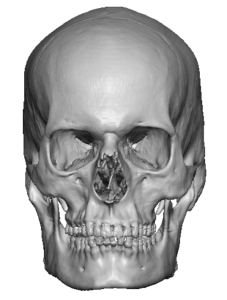


 Infraorbital rim: 2–3 mm
Infraorbital rim: 2–3 mm Maxilla: 4–6 mm
Maxilla: 4–6 mm