Midface retrusion may be corrected through either skeletal augmentation (implant-based reconstruction) or skeletal repositioning (orthognathic advancement). Although both approaches can increase midfacial projection, they differ fundamentally in biomechanical mechanism, load transmission, soft tissue response, and occlusal impact.
Analyzing the structural, functional, and biomechanical distinctions between these two strategies allows for good clinical decision making in aesthetic and reconstructive midface surgery.
Fundamental Mechanical Differences
Implant-Based Augmentation
- Adds volume anterior to existing bone
- Does not reposition the maxilla
- Occlusion remains unchanged
- Skeletal loading patterns largely preserved
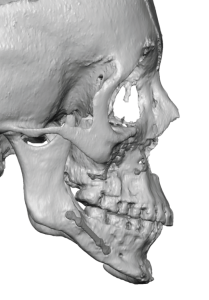
- Repositions the midface skeleton anteriorly
- Alters occlusion
- Redistributes masticatory forces
- Changes skeletal loading vectors
In essence:
- Implants = Additive projection
- Orthognathic surgery = Translational repositioning
Structural Biomechanics
1. Load Transmission
Implant Augmentation
- Load is transmitted from soft tissue through implant to underlying bone
- Masticatory forces remain native
- No change in buttress mechanics
- Implant acts as a passive contour modifier
The midface buttress system (zygomaticomaxillary, nasomaxillary, pterygomaxillary) remains structurally unchanged.
Implants do not participate in dynamic load transfer.
Orthognathic Advancement
- Altered buttress alignment
- Modified occlusal force vectors
- Redistribution of masticatory loading
- Skeletal fixation plates bear transitional load
The repositioned maxilla becomes a new load-bearing structure in altered spatial orientation.
This fundamentally changes facial biomechanics.
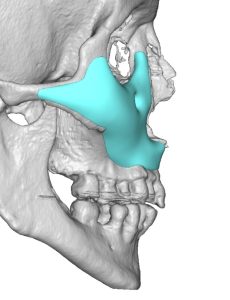
2. Buttress System Considerations
The midface functions as a vertical and horizontal buttress framework:
- Zygomaticomaxillary buttress
- Nasomaxillary buttress
- Pterygomaxillary junction
Implant Approach
- Does not modify buttress relationships
- Structural integrity unchanged
- Purely aesthetic projection increase
Orthognathic Approach
- Reorients buttresses
- May improve or destabilize depending on fixation
- Alters stress distribution patterns
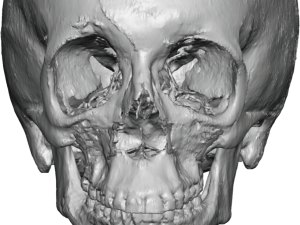
Soft Tissue Biomechanics
Implant Augmentation
Soft tissue is expanded anteriorly without skeletal translation.
Effects:
- Increased convexity
- Improved lower eyelid support
- Minimal tension shift
- No occlusal muscle reorientation
Risk:
- Overexpansion in thin skin
- Shelf effect if projection too focal
Soft tissue displacement is passive and localized.
Orthognathic Advancement
Soft tissues translate with skeletal movement.
Effects:
- Upper lip advancement
- Nasal base widening
- Nasolabial angle change
- Increased alar flare
- Altered smile dynamics
Soft tissue movement is global and tension-altering.
Occlusal and Functional Implications
Implant-Based Approach
- No occlusal change
- No orthodontic requirement
- No alteration in airway
- No mandibular compensation required
Primarily aesthetic correction.
Orthognathic Advancement
- Occlusion altered intentionally
- Requires orthodontic planning
- May improve airway in some cases
- Alters mandibular relationship
Primarily functional and structural correction.
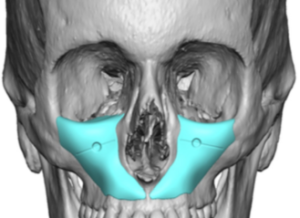
Projection Control
Implant-Based Augmentation
Projection can be:
- Differentially zoned
- Precisely mapped (2–6 mm typical ranges)
- Asymmetric when required
- Gradually feathered
Allows controlled topographic shaping.
Orthognathic Advancement
Projection magnitude determined by:
- Occlusal relationship
- Surgical advancement limits
- Vascular considerations
- Stability thresholds
Less granular control of localized projection zones.
Stability Analysis
Implant Stability
Depends on:
- Accurate pocket dissection
- Screw fixation
- Soft tissue pressure balance
Long-term stability generally high when:
- Adequate fixation used
- No infection
- Proper design prevents micromotion
Does not rely on bony healing.
Orthognathic Stability
Depends on:
- Bony healing
- Fixation plate integrity
- Postoperative orthodontics
- Neuromuscular adaptation
Relapse risk influenced by:
- Magnitude of advancement
- Soft tissue tension
- Patient compliance
Risk Profile Comparison
|
Parameter |
Implant-Based |
Orthognathic |
|
Surgical Invasiveness |
Moderate |
High |
|
Operative Time |
Shorter |
Longer |
|
Occlusal Change |
None |
Yes |
|
Relapse Risk |
Low |
Moderate |
|
Nerve Risk |
Infraorbital |
Infraorbital + others |
|
Swelling Duration |
2–6 weeks |
6–12 weeks |
|
Recovery Complexity |
Moderate |
Significant |
Indications Based on Biomechanics
Implant-Based Reconstruction Appropriate When:
- Occlusion is normal
- Deficiency is aesthetic rather than functional
- Mild-to-moderate retrusion
- Desire for localized projection enhancement
- Thin skeletal concavity without bite discrepancy
Orthognathic Advancement Appropriate When:
- Class III malocclusion
- Significant occlusal disharmony
- Severe skeletal retrusion
- Airway compromise, obstructive sleep apnea
- Functional instability
Combined Approaches
In select cases:
- Orthognathic advancement corrects occlusion
- Custom implants refine contour
This hybrid approach is common in severe congenital hypoplasia or syndromic deformities.
Energy and Force Considerations
Implants do not alter:
- Muscle vector orientation
- Bite force mechanics
- Temporomandibular joint loading
Orthognathic surgery modifies:
- Masticatory force direction
- Lever arm length
- Facial height relationships
Thus, orthognathic surgery is biomechanically transformative, while implants are structurally additive.
Long-Term Structural Implications
Implants:
- Do not stimulate bone remodeling
- Do not change craniofacial growth patterns
- Maintain original skeletal mechanics
Orthognathic procedures:
- May induce adaptive remodeling
- Alter stress shielding patterns
- Change long-term load distribution
Aesthetic Predictability
Implants:
- Highly predictable zonal control
- CAD/CAM customization
- Immediate contour visualization
Orthognathic:
- Dependent on soft tissue adaptation
- More variable aesthetic response
- Occlusion-driven movement limits contour precision
Decision-Making Algorithm
- Evaluate occlusion.
- If abnormal ? orthognathic considered.
- If normal ? implant preferred.
- Determine magnitude of retrusion.
-
- Mild to moderate ? implant.
- Severe with functional impact ? orthognathic.
- Assess patient goals.
-
- Aesthetic contour ? implant.
- Functional correction ? orthognathic.
Conclusion
Implant-based midface augmentation and orthognathic advancement are not interchangeable procedures.
They differ in:
- Mechanical mechanism
- Load distribution
- Functional impact
- Recovery profile
- Aesthetic precision
Implants provide precise, localized, structurally additive correction without altering occlusion or buttress mechanics.
Orthognathic advancement repositions the skeletal framework, redistributes load vectors, and corrects functional occlusal disharmony.
Proper selection depends on distinguishing aesthetic skeletal deficiency from functional malocclusion.
Dr. Barry Eppley
Plastic Surgeon



