
In an excellent article in the May 2008 issue of the journal Plastic and Reconstructive Surgery, these basic issues were reviewed. In HIV positive patients, they can safely undergo elective plastic surgery provided that a thorough preoperative workup has been performed. Patients with CD4 counts greater than 200 and low viral loads have surgical risks that are similar to the general population. There is no evidence to support the historic contention that they have poor or compromised wound healing. Increased surgical risks are in those patients whose CD4 counts are less than 200 or have viral loads greater than 10,000. The risk of disease transmission to the surgical team is not precisely known but is estimated to be around 0.3% for penetrating injuries from surgical sharps, a rate that is less than 10% that of hepatitic C exposure which is far more dangerous.
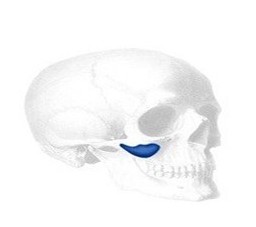
In my practice, I generally see known HIV-positive patients for facial lipoatrophy of the cheek and temple areas and fat accumulation of the back of the neck (buffalo hump). Both of these can be managed by non-surgical options although I find the surgical alternatives to give superior results. Injectable fillers, such as Scuptra, Radiesse, and ArteFill can be used to correct the typical patterns of facial wasting but they do require large volumes of injectate and numerous sessions. They quickly become as costly as surgery.
I have found performing plastic surgery on HIV positive patients to be rewarding and well appreciated. They often suffer the stigmata of their disease and wish its improvement to improve their self-esteem and improved social acceptance. I have seen no greater incidence of complications in this patients than any other types of patients.
Dr. Barry Eppley
Indianapolis, Indiana


