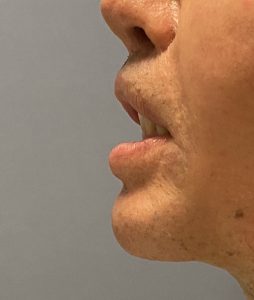
Getting the chin pad back up and achieving lip competence is a difficult challenge and numerous strategies have been advocated to do so…with varying degrees of sustained success. I have come to learn that a five level approach to chin pad repositioning, incorporating many of the known methods, needs to be considered in each patient. Not every patient will need all five levels of support and resttachment but some will.





A comprehensive approach to chin pad ptosis and lower lip incompetence requires consideration of different levels of support and suspension. Rarely does ever one level of support work to raise the lower lip and almost always three or more levels are needed for a satisfactory level of improvement.
Dr. Barry Eppley
Indianapolis, Indianapolis