The surgical placement approach for jaw angle implants is intraoral through posterior vestibular incisions. While there are some indications, and sometimes patient requests for an external transcutaneous incisional placement method, this is the rare exception to the intraoral method even if it is a safe and effective technique.
Jaw angle implants are done under general anesthesia. Patients do sometimes request a local anesthetic but this will undoubtably lead to inadequate pocket dissection and implant malposition. Ideally a nasoendotracheal tube is used but this may not be possible based on other concurrent procedures being done. (e.g., rhinoplasty)
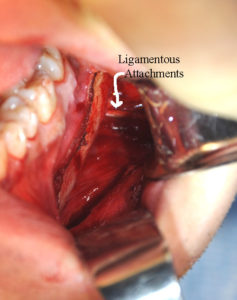
The outline of the existing jawline should be marked preoperatively. Once under anesthesia, the intraoral vestibular incision should be infiltrated with 1% lidocaine with 1:100,000 epinephrine solution. External infiltration through the skin down to the bone with subperiosteal ballooning of the tissues over the angles is also helpful. The mucosal incision should be made lateral to the vestibule opposite the molar teeth to keep a buccinator muscle tissue cuff to aid in closure. The long buccal neurovascular bundle is frequently encountered and is retracted medially. Once on the bone at the external oblique ridge, wide subperiosteal undermining is done back to the posterior border, superiorly to the coronoid notch, down to the inferior border and anteriorly up under the incision along the inferior border. There is no reason to have a limited pocket dissection which is the primary cause of inadequate jaw angle implant positioning and asymmetry. However the gentle elevation of the pocket, particularly inferiorly and posteriorly, is necessary. The use of a J-shaped or curved elevator is helpful in this regard.
Once adequate pocket dissection is done, implants sizers should be used for try ins to determine the extent of pocket creation and the effect of implant size. Equally relevant, sizers limit dragging the actual implant to be placed through the mouth to one time. In doing so this is a valuable step in decreasing the risk of implant bacterial inoculation and developing a postoperative infection.
Positioning of the implant at the jaw angles is theoretically ‘easy’ when viewing it from an implant sitting on a skeletal model. However in the back recesses of the mouth where the back end of the implant can not be seen that well as to where it sits relative to the actual bony angle, it is far more challenging. Asymmetry of jaw angle position is not rare between the two sides because of this limited visual assessment. While the implant designs on their inner surface may seem like they will simply ‘lock into place’ when adequately positioned, this does not occur.
Once the jaw angle implant is positioned as desired, I consider screw fixation to be essential. While the fixation of facial implants everywhere else can be debated, it is crucial in jaw angle implants. Neither the implant shape or pocket dissection can be counted on to control after surgery the desired implant location on the bone. Screw fixation in my experience is essential.

Meticulous closure of the incisions in the back of the mouth is critical to avoid postoperative wound dehiscence, implant exposure and infection. A two layer closure is done with a running 3-0 Vicryl suture for the muscle and a running 3-0 chromic suture for the mucosa.
Dr. Barry Eppley
Indianapolis, Indiana



