
In the May issue of the Aesthetic Surgery Journal, the effect of incision choice on outcomes in breast augmentation were evaluated. Out of Georgetown University in Washington DC, a study of nearly 200 primary breast augmentation cases over a six year period was reported. These were on initial breast augmentation patients who received an implant only and had no other procedure such as a lift. The patients had to receive round breast implants and not shaped implants, regardless of whether they were saline or silicone devices. A total of 336 augmented breasts comprised the study.
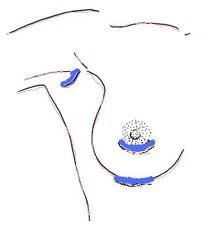
The postoperative complications that occurred were capsular contracture (1.8%), hematoma (0.9%) and infection (0.3%) amongst all patients. Use of a transaxillary incision was associated with the highest incidence of capsular contracture (6.4%) compared to the periareolar (2.4%) and inframammary crease.(0.5%) The authors conclude that the risk of capsular contracture is significantly higher and statistically significantly different than with periareolar or inframammary fold incisions.
The significance of this study to me has several take home points. First, it illustrates and reinforces that there are real risks with an implant-driven operation like breast augmentation. While it is an exciting and often dramatic image-improving operation for most women, it is not complication free. Complications such as those evaluated in the study do occur and they are not rare. Second, the inframammary incision is associated with the lowest risk of certain complications particularly capsular contracture. Why? Because it allows direct access to the release of some of the inferior attachments of the pectoralis muscle. Inadequate muscle release accounts for persistent high positioning of the implant and inadequate pocket release and size for the implant.
Having done a lot of saline breast augmentations through the transaxillary approach prior to the re-introduction of silicone in 2006, occasional problems were seen with inadequate lower pocket development. Switching to the inframammary approach with the return of silicone, most of these problems no longer occur. Even with using saline implants today, I prefer to access and develop the pocket from below. I feel the results are significantly better with improved implant symmetry and positioning.
While some patients understandably want to avoid any visible scars on the breast, it is important to remember that the operation is ultimately about the implant not the incision. With today’s funnel insertion technique, even a large silicone implant can be inserted through a fairly small inframammary fold incision.
Dr. Barry Eppley
Indianapolis, Indiana


