Background: Access to the brain and its lining requires the removal of part of he skull. Known as a craniotomy flap, the bone is usually removed in he shape of a semicircle or a full circle. Once the intracranial work is complete the bone flap is put back into place. But because the bone edges are vertical and a thin rim of bone at its perimeter has been removed in its creation, such bone flaps are well known to fall in or sink down creating an external bone contour deformity of the skull.
To avoid craniotomy flap sinking, plate and screw fixation is commonly used. A variety of differently shaped plates have been developed to rigidly hold the bone flap up as it heals. But despite such metal fixation, not all bone flaps always stay up as much as desired usually due to the failure of good bone healing across the surrounding bone flaps.
Treatment of a depressed craniotomy bone flap can be done by two fundamental approaches…either reposition the bone flap or leave it in place and contour on top of it. Both methods can be effective but employ very different technologies to perform.
Case Study: This middle-aged male had a left temporal craniotomy performed due to a traumatic injury and the need for treatment of a subdural bleed. Six months after the procedure, he had a very noticeable temporal depression that made him look like a piece of his head was missing from certain angles. The anatomy of his temporal depression was more than just the sinking of the bone flap, it was also due to the atrophy of the temporalis muscle as well.

Highlights:
- Temporal craniotomy bone flaps can become depressed despite rigid fixation.
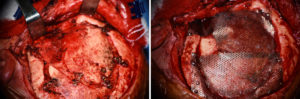
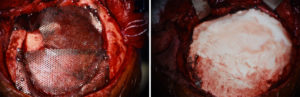
- One approach to craniotomy flap reconstruction is to leave the depressed bone flap in placed and build out the contour to the level of the surrounding bone.
- The combination of hydroxyapatite cement and a mesh floor can be used to augment a depressed craniotomy bone flap.
Dr. Barry Eppley
Indianapolis, Indiana