Background: Facial fractures are common and can be repaired by a variety of bone repositioning and fixation methods. But despite good bony realignment the fullness and projection of the traumatized facial areas do not always return not normal. Between the trauma of the original injury and that of the subsequent facial fracture repair, soft tissue changes do occur. Fat loss occurs and scar tissues pull inward creating atrophic soft tissue changes over and around the facial fracture site. The bigger the original facial trauma was the more extensive these soft tissue changes will be.
Such soft tissue changes are most significant in the midface that has sustained fractures. This is because the soft tissues of the midface are often thinner in many patients and the bones (maxilla and pyriform aperture area) have a natural concave profile to them. Restoration of the bony alignment through the re-estabishment of the occlusion and the wound conjecture that results can create still result in a pan facial deficiency profile.
Loss of soft tissue projection of the midface can be treated by several methods. Fat injections can be done but this is more effective in the sides of the face than around the nose and upper lip. Building up the maxillary and nasal base area can be done by a variety of onlay materials from bone grafts, hydroxyapatite granules and cements, to synthetic materials.
Case Study: This middle-aged female sustained severe and multiple facial fractures (mandible, maxillary and cheek-orbital fracture from a motor vehicle which underwent primary repair at the time right after the original injury. She was referred six months later with a Class III malocclusions and a dish face appearance. (panfacial deformity) She subsequently underwent a LeFort I octetomy advancement which corrected her occlusion and improved her midface projection somewhat. But she remained with inadequate midface projection of the central and lateral face (her cheekbones had good projection) and her face appeared sunken.
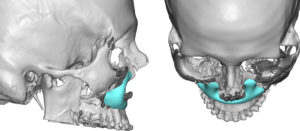

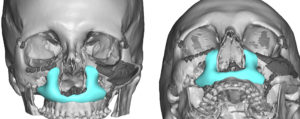
The treatment of soft tissue atrophy of the midface often requires a superficial and deep approach. In the properly selected patient building up the bone around the pyriform aperture can be done with a custom midface implant approach. It offers assured projection and volume retention that is designed to add symmetric augmentation based on the underlying bone shape.
Highlights:
1) Bone restoration of facial fractures will not always restore pre-injury facial projection.
2) Loss of facial projection can occur from subcutaneous tissue atrophy and scar .
3) Injectable fat grafting and bone-based augmentation with implants are the treatment options for improving the projection of the dramatically recessed midface.
Dr. Barry Eppley
Indianapolis, Indiana