Background: Gynecomastia is a common male problem that affects men of all ages. While it is most commonly recognized in teenagers after puberty, it actually affects middle-aged and older men almost as frequently…and often not less aesthetically bothersome. The older man with obvious breast tissue jiggling in their shirt is a well known phenomenon that is quite easy to find.
When gynecomastia becomes significant, the enlarged breast tissue creates a visible mound. If it is large enough or in an older man where the chest skin is more lax, an actual breast ptosis can occur. This is where the breast mound actually hangs off of the chest wall laying on or over the inframammary fold. While this is bothersome enough for a woman, it is particularly unsettling in a man. No amount of weight loss or exercise will solve this significant ‘man boob’ problem.
The most frequently used gynecomastia surgery techniques include liposuction of all types and open excisions done through an areolar incision. But this more advanced degree of gynecomastia is not going to be corrected by even a combination of areolar excision and liposuction. This is because neither can adequately treat a significant part of the gynecomastia problem…extra or loose skin.
Case Study: This is a 47 year-old male who wanted to get rid of his ‘breasts’. He was also an athletic male who used to work out a lot but had not done so over the past several years. He had gained weight, he developed breasts and his chest dropped. This was a great source of embarrassment for him.
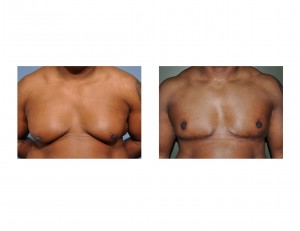
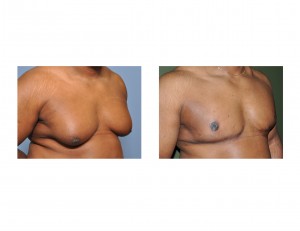
Gynecomastia surgery that includes wide horizontal excision and nipple-areolar transposition is one of the most extensive treatment methods. But when a large and hanging breast mound exists, this is the only effective approach. While it involves bigger incisions, the recovery time is not much longer than most other gynecomastia surgeries.
Case Highlights:
1) Large gynecomastias that involve breast mounds that hang off of the chest wall with a low nipple position will not respond to traditional gynecomastia treatment methods.
2) Breast tissue and skin must be removed but traditional breast reduction methods in men introduce unacceptable amounts of chest scarring.
3) A horizontal excision of breast tissue and skin with superior nipple transposition can effectively lift and flatten the chest with an acceptable scar location and a preserved nipple in large male gynecomastias.
Dr. Barry Eppley
Indianapolis, Indiana


