Background: Lip augmentation has been a facial aesthetic procedure that has been done by non-surgical and surgical methods for many decades. While it is done mainly today by injectable fillers or fat injections, a permanent implant approach has also been done both historically as well as today. Over this time period different materials have been used for lip implants with variable success.
Implants placed in the lips must fulfill unique criteria that are different than any other form of facial implant. Because the lips are soft and supple, subject to frequent motion and are in a facial area of high sensitivity, any implant material put into the lips must be similarly very soft and flexible. The only lip implant available today (Permalip) is made of an ultrasoft silicone and is the best implant material every used in the history of implant lip augmentation. While it is not perfect and has its share of aesthetic complications it has about the most softness and suppleness that any implant material could offer. But it also offers one desirable feature that to many seems counterintuitive but is always an important implant feature on the face or body…easy reversibility.
But the history of lip implants has not always had materials used that fulfill many of these desirable qualities. One such implant material was a perforated ePTFE implant. The concept seems logical with a soft tube of ePTFE with a hollow center into which tissue ingrowth would provide an ‘auto’ implant that was soft and supple and provided permanent volume. While well intentioned and seemingly made good biologic sense the clinical reality was very different.
Case Study: This middle-aged female had a ‘Gore-tex’ implant placed for lip augmentation and support of a congenital lower lip malformation over twenty years previously. She had never liked it as it felt stiff and gave her periodic discomfort. It felt irregular and immobile.

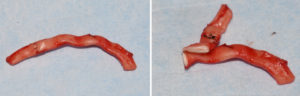
The lip is a tough place for any implant to function because no material can ever have the exact feel and suppleness of natural lip tissue. Because all such implants develop an encapsulating scar this adds to its potential firmness as well as potential lip distortion. It is for this reason that any lip implant material be just as easily reversed by the same technique by which it is inserted. If the lip implant develops a lot of tissue adherence it will have to be removed by an open approach as in this patient example.
Highlights:
1) Certain types of lip implants used in the past have tissue ingrowth and their removal requires an open approach.
2) One very effective incisional approach is a vermilion-cutaneous incision for lip implant removal which provides direct access to remove the implant intact as well as its surrounding capsule.
3) The scar from the vermilion-cutaneous incision in lip implant removal heals in an imperceptible fashion in most patients.
Dr. Barry Eppley
Indianapolis, Indiana



