Background: Most frontal sinus problems can be successfully managed with an endoscopic approach. But if frontal sinus drainage can not be successfully established, an open approach for its treatment may be needed to eliminate the entire frontal sinus.. The osteplastic bone flap approach for frontal sinus obliteration has been around for a long time to treat such problems as chronic frontal sinusitis, mucopyoceles frontal sinus tumors and frontal sinus fractures that involve the posterior table.
In frontal sinus obliteration there are three key manuevers, complete removal of all sinus lining, sealing of the frontonasal duct and filling in of the entire frontal sinus. The only variable historically has been what material to opacify the frontal sinus. Historically it has been the use of autologous fat. But hydroxyapatite cement was introduced in the 1990s and offered an off the shelf material that did not require a fat graft harvest. Hydroxyapatite cement has the potential to osteointegrate into the surrounding bone and provides a stable contour to the frontal forehead area.
Regardless of the material used, the key to success in frontal sinus obliteration is the complete removal of mucosa and obliteration of the frontonasal duct. No implanted material will be successfully of residual mucosa remains which can ultimately become a source of chronic pain and/or a mucoceole.
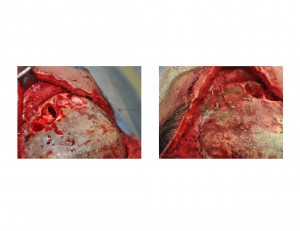
Case Study: This 35 year-old female had a history of frontal sinus obliteration which was needed because of infection that developed after an open brow bone reduction procedure. She had chronic pain over the central sinus area that persisted for several years. A CT scan showed a radiolucent cystic area under the brow bone area where her pain was. She requested that the hydroxyapatite cement be removed and replaced with cranial bone grafts.
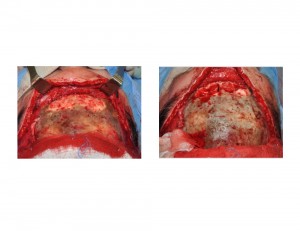
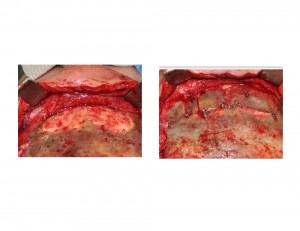
Secondary frontal sinus obliteration can be done using cranial bone grafts after removal of hydroxyapatite cement. A smooth outer brow bone contour can be obtained with careful shaping and adaptation of monocortical cranial bone grafts. Any small defects in the gaps can be filled with demineralized bone paste.
Case Highlights:
1) Obliteration of the frontal sinus with hydroxyapatite cement is an alloplastic method that is historically very successful.
2) Hydroxyapatite cement can be removed from the frontal sinus and replaced with autogenous bone grafts
3) Reconstruction of split thickness cranial bone graft sites can be done with hydroxyapatite cement.
Dr. Barry Eppley
Indianapolis, Indiana