Background: A webbed neck, medically known as pterygium colli deformity, is a well known but rare congenital neck condition. Skin folds are present along the sides of the neck from the back of the head behind the ears down to the shoulders. The hairline often follows the skin folds in their upper part. It is most commonly seen in Turner’s syndrome but occurs on congenital syndromes as well. The skin folds occur in varying presentations but can be quite pronounced in many cases.
The surgical correction of the webbed neck has evolved from original descriptions of z-plasties done directly along the skin folds. While successfully breaking up the skin folds, such a direct approach leaves unsightly scars that are rarely worth the trade-off.
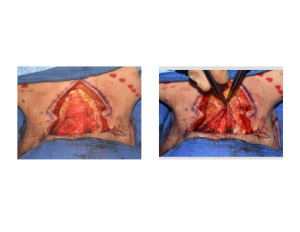
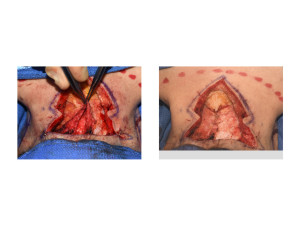
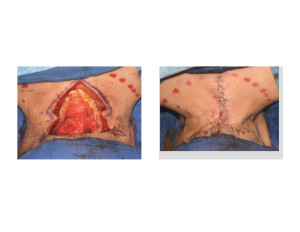
The posterior approach to the webbed neck is the preferred technique today. This involves removing tissue from the midline of the posterior neck and wide skin undemining out to the skin folds. Closing the posterior neck defect then pulls the skin folds inward. (more posteriorly) A variety of posterior neck excisional patterns have been described from butterfly, M and Z-plasty patterns. While providing definite improvement in the appearance of the skin folds and keeping the scar fairly hidden (with long hair), partial relapse is common with the secondary skin relaxation.
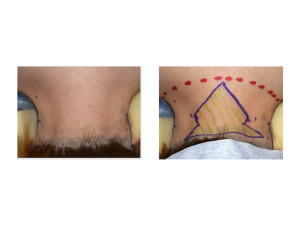
Case Study: This 35 year-old Asian female had a congenital webbed neck from birth. She did not have Turner’s or any other known congenital condition. Her necks webs would be described as mild to moderate. She was teased a lot for her neck webs when she was growing up. Prior to surgery, she shaved the lower portion of her occipital hairline to aid the subsequent surgery.


Highlights:
1) Webbed neck correction requires a posterior neck approach with tissue excision and midline closure to prevent visible scars on the sides of the neck.
2) Midline fascial plication is critical to bring in the sides of the neck (webs) and relieve tension on the posterior midline neck closure.
3) This form of webbed neck surgery uses the same principles as midline platysmal plication in facelift or direct anterior necklift surgery.
Dr. Barry Eppley
Indianapolis, Indiana




