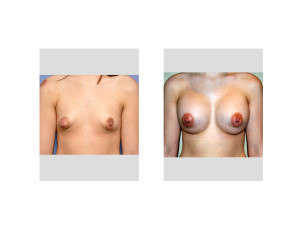
Tuberous breasts are a well known congenital breast problem that presents in varying degrees of deformity. It has its greatest impact with the patient who presents for breast augmentation and often adjunctive strategies must be done at the time of implant placement to get a good breast shape result. Women often recognize that their breast(s) are misshapen but don’t know the exact name of the deformity.
Tuberous breasts are characterized by a breast base constriction (narrow diameter), small breast development, a high inframammary fold and inferior pole skin shortage and the classic areolar herniation presentation. Since it presents as a spectrum of deformity several classification systems have been devised which can be used to help with matching the deformity with the type of corrective breast procedure needed.
In the January 2015 issue of the journal Plastic and Reconstructive Surgery the article entitled ‘Tuberous Breast Deformity: Classification and Treatment Strategy for Improving Consistency in Aesthetic Correction’ was published. Using 26 patients (51 breasts) a three-tiered classification system was used based on the degree of base constriction, level of the inframammary fold, breast volume, amount of skin envelope, degree of ptosis and amount of areolar herniation. What differentiates their classification system are the added descriptors of ptosis and areolar herniation. The surgical technique included periareolar incisions, glandular dissection down to the level of the new inframammary fold, radial scoring of the inferior dermoglandular flap, submuscular release and dual plane tissue expander or implant placements. Circumareolar lifts are performed lastly to correct ant ptosis and enlarged areolas.
Of the tuberous breasts treated, 12 type 1, 26 type 2 and 13 type 3s were treated. MOst patients (92%) had a one-stage correction while a two-stage approach using a tissue expander was needed in the remaining 8%. A periareolar mastopexy was used in almost every patient (96%) with the addition of a vertical mastopexy in a limited few. (8%) Few complications occurred (8%) which were capsular contractures or implant malposition.
This article provides a logical and thoughtful approach to the treatment of tuberous breasts that can be done as a single stage correction in most cases.
Dr. Barry Eppley
Indianapolis, Indiana


