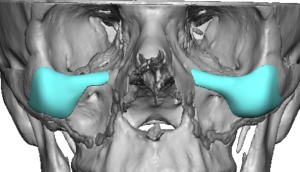
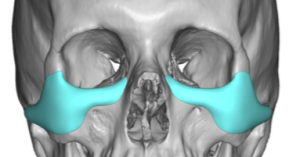
Custom implant designs offer great versatility for augmentation of upper midface aesthetic bony deficiencies particularly the undereye area. There are two basic types of undereye custom designs, infraorbital (IO) and infraorbital-malar (IOM) implants. A comparison of infraorbital-only versus infraorbital–malar implants, focusing on when each works, when it doesn’t, and why, will make the difference in successful or inadequate undereye work.
Core difference in one sentence
- Infraorbital-only implants correct the rim,
- Infraorbital–malar implants correct the rim + the supporting platform beneath the lower lid.
That second part is the game-changer.
Anatomical Coverage
|
Feature |
Infraorbital-only |
Infraorbital–malar |
|
Infraorbital rim |
? Yes |
? Yes |
|
Tear trough |
?? Partial |
? Yes |
|
Anterior malar support |
? No |
? Yes |
|
Lower lid vertical support |
Minimal |
Significant |
|
Midface vector correction |
? No |
? Yes |
Aesthetic effect

 Infraorbital-only
Infraorbital-only
What it improves
- Sharp rim definition
- Mild hollowing near the orbital margin
- Subtle smoothing of the tear trough
What it doesn’t
- Lid–cheek junction remains visible
- Hollow reappears when smiling
- Doesn’t support thin lower lids
- Can look “rim-heavy” in animation
Best described as edge correction without foundation correction.

 Infraorbital–malar
Infraorbital–malar
What it improves
- Continuous lid–cheek transition
- True tear trough elimination
- Lower lid support (less scleral show risk)
- Smooth transition into the malar augmentation
- An upper midface contour effect
- The augmentation effect can extend out into the zygomatic arch sutural line and beyond if desired.
This is platform correction, not edge camouflage.
Risk profile
Infraorbital-only risks
- Visible rim step-off
- Lack of adequate rim projection
- Inadequate correction ? revision
- Persistent tear trough despite implant
Infraorbital–malar risks
- Underprojection if indequate design
- Excessive fullness at the infraorbital-malar junction
- Edging at medial infraorbital rim or end of zygomatic arch
- The complication risk isn’t higher—but with a larger surface area coverage design error risks are higher.
Surgical considerations
|
Factor |
Infraorbital-only |
Infraorbital–malar |
|
Incision |
Transconjunctival or subciliary |
Subciliary |
|
Dissection |
Limited |
Extended subperiosteal |
|
Fixation |
Needed |
Needed |
|
Operative time |
Shorter |
Longer |
|
Revision ease |
Easy |
Easy (silicone) |
The surgical difference is modest—the planning difference is not.
Ideal indications
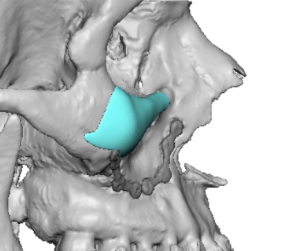
- Deficiency is isolated to the rim
- Patient has adequate malar projection or only some anterior malar projection but no lateral malar augmentation
- Tear trough is shallow and static
- Lower lid tone is excellent
These indications are uncommon.
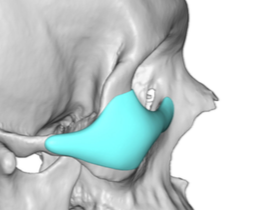
- Tear trough is deep or dynamic
- Negative or flat midface vector
- Hollowing appearance is profound indicating a malar deficiency as well
- Filler or fat injections barely made any improvement
- Herniated lower lid fat pads are present
This is the majority of true undereye hollowing patients.
A useful rule of thumb
If you’re tempted to add filler below an infraorbital implant—
you should have done an infraorbital–malar implant instead.
Bottom line
- Infraorbital-only = niche, limited, often underpowered
- Infraorbital–malar = anatomically correct solution for real undereye hollowing
Most “failures” of infraorbital implants are not material or surgical problems—they’re insufficient implant footprint.
Dr. Barry Eppley
World-Renowned Plastic Surgeon




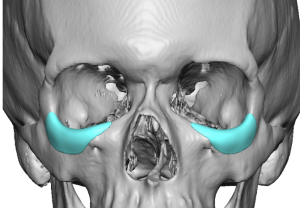
 Infraorbital-only
Infraorbital-only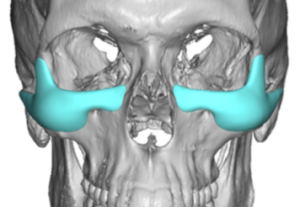
 Infraorbital–malar
Infraorbital–malar