Buttock implants today are becoming increasingly done using the intramuscular technique. While this implant is better long-term due to an increased well vascularized soft tissue cover, it is not complication free. It is still exposed to potential infection, hematoma and seromas like the subfascial implant location…although at a much lower rate.
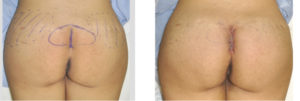
In the January 2015 Global Open issue of the journal Plastic and Reconstructive Surgery, a paper entitled ‘Case Study: Reduction of Gluteal Implant Infection Rates with Use of Retention Sutures’. To prevent the intergluteal wound incision, the authors used a simple closure technique combined with intramuscular gluteal implantation to help reduce tension and wound dehiscence and ultimately lower infection rates. After intramuscular implant placement, a three layer closure was used, 0 Monocryl in the gluteal fascia, 2-0 Monocryl in the dermis, and 3-0 chromic simple running stitch in the skin layer. Final layer of closure of the gluteal flap included the use of retention sutures of 2-0 nylon tied over 2-cm pieces of silicone tubing cut from Jackson Pratt drains along the sacral incision. Drains were removed after one week. The retention sutures were removed at three weeks. Patients returned to full activities at six weeks. In three patients treated with this closure technique they all healed uneventfully.
There is little question that having a competent intergluteal incisional closure will help reduce complications from buttock implants. Different surgical wound closure techniques can be used, and they all can be successful, as long as great effort is protect the skin incision against postoperative shearing forces. The technique described in this paper is a good one and will be as successful as any. I use an additional suture layers between the gluteal fascia closure and the dermis to quilt down the dead space from the subcutaneous dissection. After dermal suturing, I use permanent horizontal mattress sutures and leave them in for weeks.
While the development of buttock implant complications can arise from many different reasons, striving to achieve an incisional closure is a simple and inexpensive technique that is withe small amount of extra operating room time to do.
Dr. Barry Eppley
Indianapolis, Indiana


