Liposuction is one of the most common and successful body contouring procedures. Having now been around for almost 35 years in the U.S., it has undergone many evolutions and refinements in treatment strategies and in the equipment to do it. With widespread use of liposuction by many different practitioners and methods, complications from liposuction surgery were inevitable. While most of these complications are more aesthetic in nature, the most serious ones are of medical origin. Complications such as infection (necrotizing fasciitis), deep vein thrombosis, pulmonary emboli and death have all occurred and have led to a variety of preventative measures for their prevention.

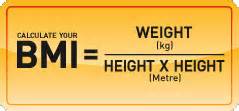
In the September 2015 issue of the journal Plastic and Reconstructive Surgery, an article appeared entitled ‘Is There a Safe Lipoaspirate Volume? A Risk Assessment Model of Liposuction Volume as a Function of Body Mass Index’. In this paper the authors analyzed over 4,500 liposuction patients from a large plastic surgery database. They identified 69 out of 4,534 patients who developed a serious postoperative complication. Interestingly 97% of the large volume liposuction procedures were done in an outpatient setting. The amount of fat removed and the body mass index of the patients were found to be significant independent risk factors for complications. They found that liposuction volumes in excess of 100ml per unit of body mass index was a good predictor of complications. Their findings indicate that traditional liposuction volume thresholds do not accurately predict the risk of complications in any one patient. Looking at the volume of fat removal in the context of the patient’s physical measurements and body surface area is a more accurate way to establish an upper limit for an individual patient.
Patient deaths from liposuction over the years has led to restrictions being limited on the amount of liposuction fat aspirates. The most common maximum liposuction aspirate is that of 5,000 liters and is widely quoted. The Patient Safety Committee of the American Society of Plastic Surgeons has even adopted this number as an important safety marker. This study shows, however, that there were no differences between large volume liposuction (greater than 5,000 liters) vs. normovolemic liposuction (under 5,000 liters) with the exception of non-life threatening seroma rates.
Dr. Barry Eppley
Indianapolis, Indiana


