Introduction
A negative orbital vector is a facial aesthetic descriptor referring to the relationship between the globe (eyeball) and the infraorbital rim/midface projection.
A negative orbital vector occurs when the globe projects further forward than the infraorbital rim and malar (cheek) bones.
In practical terms:
?? The eyes sit farther forward than the supporting bone beneath them.
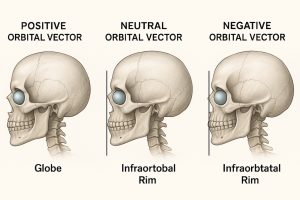
- If the infraorbital rim sits behind this vertical plane ? negative orbital vector
- If it lies on or in front of the plane ? neutral or positive vector
Clinical Relevance
A negative orbital vector reduces the structural support of the lower eyelid, contributing to:
- Lower lid laxity
- Undereye hollows or depression
- Scleral show (visible white beneath the iris)
- Increased risk of eyelid retraction or ectropion after surgery
- Higher-risk profile for lower blepharoplasty
Aesthetically, it may present as:
- Prominent or “large-appearing” eyes
- Tear trough deformity
- Infraorbital hollowing
- Malar deficiency or midface retrusion
I frequently reference orbital vector analysis during treatment planning for:
- Custom infraorbital and midface implants
- Pseudo-exophthalmos concerns
- Strategies for improving lower eyelid support and periorbital balance
Etiology
Common anatomical contributors include:
- Midface hypoplasia (congenital or ethnic variations)
- Infraorbital rim deficiency
- Prominent globes (e.g., increased axial length, thyroid eye disease)
- Variations in orbital/facial skeletal growth
Treatment Options
Non-Surgical
- Tear trough and infraorbital fillers
- Malar/cheek fillers
These modalities improve contour but do not correct the underlying skeletal deficiency.
Surgical
- Custom infraorbital or orbital rim implants — most effective structural treatment
- Fat grafting (limited effectiveness in true vector deficiency)
- Canthopexy or canthoplasty for eyelid support
- Midface advancement in severe skeletal deficiencies
Case Study
A young male presented with:
- Significant undereye hollows
- Rounded lower eyelid shape
- Pronounced scleral show
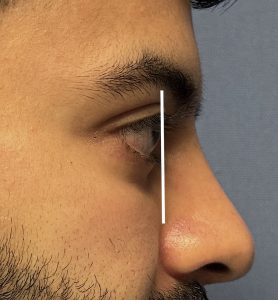
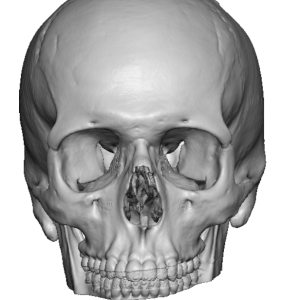
Imaging Findings
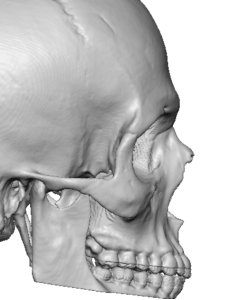
- Marked infraorbital rim recession
- Increased orbital height (supraorbital-to-infraorbital distance)
- Rounded infraorbital rim contour
These features are classic for a negative orbital vector.
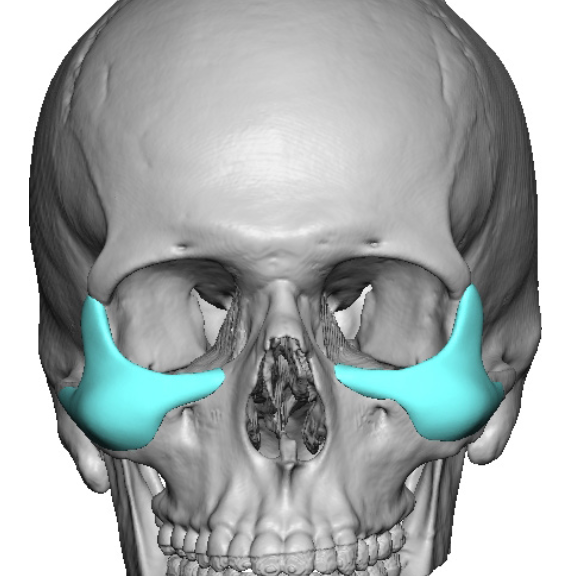
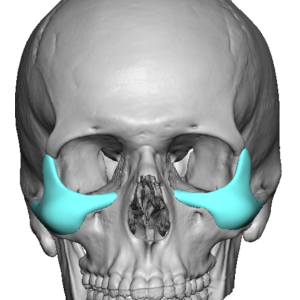
Implant Design
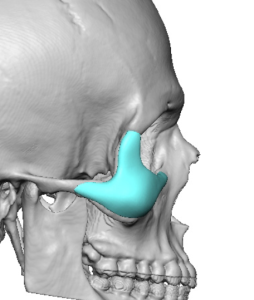
- Infraorbital rim augmentation
- Lateral orbital wall extension
- Zygomatic (malar) enhancement
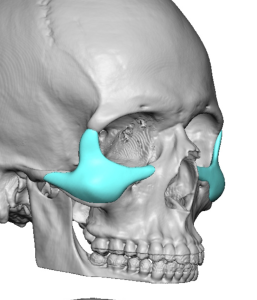
Surgical Technique

- A broad subperiosteal pocket was developed from nasal bones to the zygomatic arch, and from the frontozygomatic suture to the inferior zygomatic buttress.
- Implants were inserted and secured with microscrews.
- Lower eyelid vertical height was increased using 10 mm AlloDerm spacer grafts, combined with a lateral canthopexy.
Discussion
Patients with a negative orbital vector have an underlying skeletal imbalance that cannot be effectively corrected with standard, preformed implants. Traditional tear trough or cheek implants have limited ability to address the complex three-dimensional deficiency.
Rationale for Custom Implantation
A custom implant should be conceptualized similarly to correcting a depressed ZMC fracture:
- In such fractures, the ZMC complex is displaced posteriorly (often inferiorly as well).
- Correction involves forward and upward repositioning—analogous to what is needed in negative orbital vector augmentation.
Therefore, tripod augmentation (infraorbital rim, lateral orbital rim, and malar region) is essential.
Raising the height of the infraorbital rim and sweeping the contour into the lateral orbital rim provides improved lower lid support and better orbital shape.
Soft Tissue Considerations
Even with ideal bony correction, the lower eyelid frequently requires adjunctive support:
- Lower lid spacer grafts
- Lateral canthal tightening or repositioning
These procedures address the soft tissue component and enhance surgical stability and aesthetics.
Key Points
- Custom infraorbital–malar implants with a tripod design are the most powerful solution for correcting the skeletal deficiency in negative orbital vector anatomy.
- Adjunctive eyelid procedures—including lower lid spacer grafts and lateral canthal support—optimize functional and aesthetic outcomes.
- This comprehensive approach can be fully performed through a subciliary incision, providing access for skeletal and soft tissue correction.
Barry Eppley, MD, DMD
World-Renowned Plastic Surgeon