Background: While many people think of the jaw when a facial structure is skeletally or structurally deficient, every other facial bone can also have visible hypoplasias as well. The orbital bones are no exception and their complex circumferential shape and the eyeball that lies within have unique clinical presentations of bony deficiencies.
While many people develop tear trough and infraorbital hollows with aging due to fat loss and tissue sagging, such clinical presentations in young people suggest another cause. It usually indicates the bone structure is weak, specifically the infraorbital rim. When this section of the orbital bone lacks adequate horizontal projection, it affects multiple adjacent structures. First the lower eyelids lack skeletal support as it can be seen to be flat with the eyeball protruding forward. This creates infraorbital hollows with a line of demarcation along the bone. This can be associated with dark circles and a tired appearance. Secondly the ’protruding’ eyeball (technically known as globe pseudo protrusion) creates the well described negative orbital vector, meaning the cornea of the eye sticks out further than the bony infraorbital rims in profile view. Lastly the anterior cheeks are often flat as well as the infraorbital-malar region develops as a combined bony unit.
Infraorbital bony recession is most commonly treated by injectable fillers or fat as a voluminization technique. But this is often associated with variable success and is prone to irregularities due to the thin tissue of the lower eyelid which is very unforgiving. Skeletal augmentation is the more effective treatment approach even if it is more invasive because it treats the actual problem. But attempting to do so often produced unsatisfying results historically as creating a smooth and complete skeletal augmentation of the area lacked a good technique to do so.

Case Highlights:
1) Infraorbital hollows caused by bony recession creates the classic negative orbital vector.
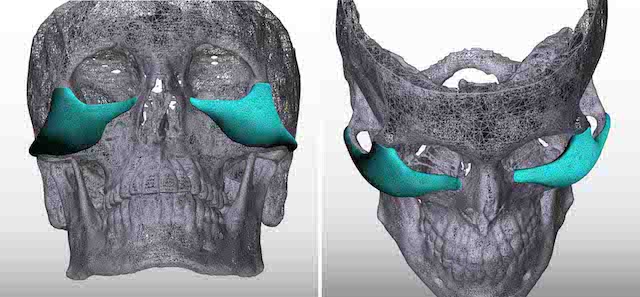
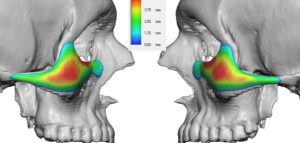
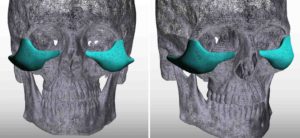
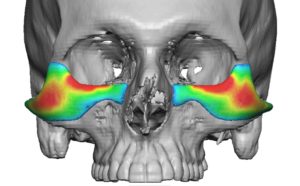
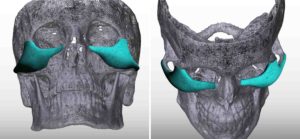
2) True infraorbital bony recession is best treated by augmenting the infraorbital rim and out onto the malar region as well as a composite augmentation approach.
3) A custom infraorbital-malar implant designed to augment the height of the infraorbital rim and the thickness of the lateral orbital rim is the most ideal approach to a addressing this orbital skeletal deficiency.
Dr. Barry Eppley
Indianapolis, Indiana