Background: Aesthetic augmentation of temporal hollowing, like most forms of facial augmentation, is most commonly done using injectable fillers and fat. This is certainly appropriate given that temporal hollowing is a soft tissue deformity and not as a result of a bone defect or deficiency. While different forms of such injectates exists and their advantages are an immediate effect and are non- to minimally surgical in nature, they also have distinct disadvantages. Most have no assured permanent volume retention and there are always potential issues with irregularities and asymmetries.
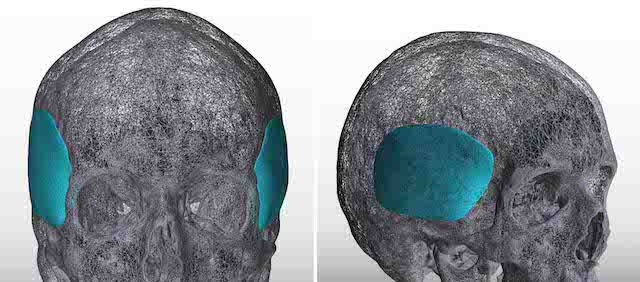
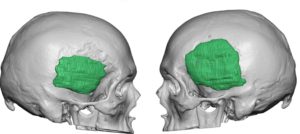
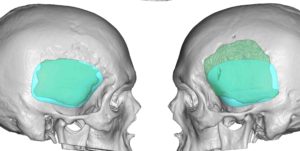
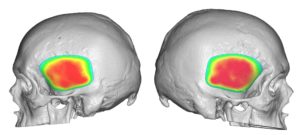
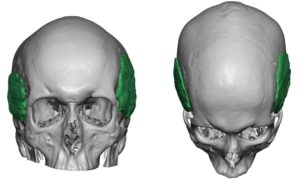
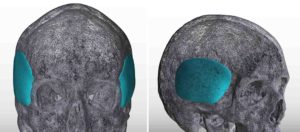
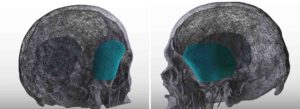
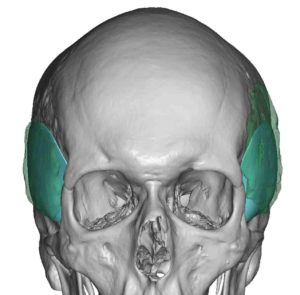
Before injectable temporal augmentation techniques came into popularity, they were done far less frequently and using bone-based methods. The implanted materials were most commonly bone cements or some form of reconstructive implant. While treating a soft tissue temporal hollowing using bone augmentation to push out soft tissues has theoretical merit, the natural angulation of the temporal fossa bone creates potential issues with it. The deepest part of temporal hollowing is where the deepest concavity of the bone is….which is difficult to fully and smoothly fill. It also requires a temporal hairline incision for access which poses its own potential aesthetic tradeoff.
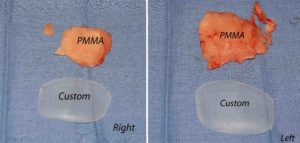
Unless it is done through fully open coronal scalp incision as part of a reconstruction, it is very hard to fill the temporal fossa in an even manner. When done for cosmetic purposes, a cranofacial approach with bone cement has been historically used through a temporal hairline incision. But like all bone cements placed through smaller incisions the risk of irregularities and asymmetries can occur. While one may think that buried under the thick temporalis muscle such irrregularities would be obscured…this is not the case.
Case Highlights:
1) Temporal augmentation can be done either by bone or muscle augmentation.
2) The traditional approach of temporal augmentation is done on the bone with various forms of bone cements which are prone to irregularities and asymmetries.
3) Custom temporal implants offer an assured smooth contour and controlled thicknesses and location of the augmentation
Dr. Barry Eppley
Indianapolis, Indiana