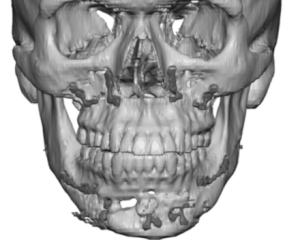
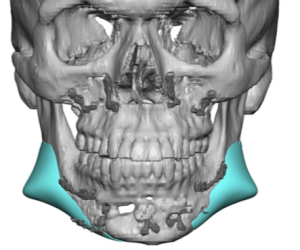
Background: The traditional approach to aesthetic jaw implant surgery is a combination of intraoral (2) and external incisions. (1) The intraoral incisions are needed to access the jaw angle region where that portion of the implants are placed on the bone under the masseter muscle. While the intraoral approach to the jaw angles is scarless, it is associated with an increased risk of infection. In addition there is also an increased difficulty in being certain of ideal implant placement due to the more limited visual access that occurs inside the mouth.
The central submental incision is usually done externally for direct access to the chin because it is in a more hidden area and usually heals well. While an external approach to the jaw angle region is commonly done in jaw fractures and in jaw reconstruction, it is rarely done in aesthetic jaw surgery due to scar concerns. But it does offer a more direct access to the bony jaw angles with direct visualization of the implant placement on the bone. Unlike the traditional neck skin incision (Risdon) which is placed on the neck in a horizontal skin crease, a more direct skin incision can be made along the jawline. Being up along the jawline the incision lies above the course of the marginal mandibular branch of the facial nerve so that is not at risk of being injured.
Jaw implants are composed of various materials, each with their own advantages and disadvantages. One of these is Medpor which has a robust tissue adherence and is a stiffer material. Its major disadvantage is when it becomes necessary to remove it. This is met with considerable resistance by many surgeons as the difficulty in doing so is considerable and is associated with its own risks in doing so. (blood vessel and nerve injury) These risks are maximized at the jawline areas behind the chin where getting the implant free along the inferior border where the neurovaccular structures cross is a significant concern.

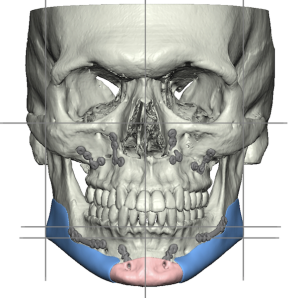
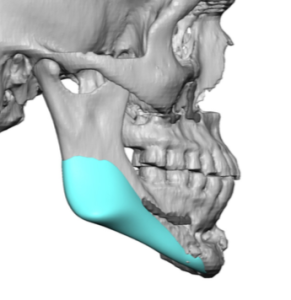



This case illustrates two important concepts. First, while Medpor implants are difficult to remove it can always be done in my experience. There are several intraoperative techniques to do so successfully. Second, the transcutaneous approach to the jawline provides direct access and in the properly selected patient the scarring may be acceptable. Its major advantage is that it avoids any intraoral incisions which lowers the risk of infection and certainly expedites the recovery processs from the standpoint of eating and oral hygiene.
Case Highlights:
1) The transcutaneous approach to jaw implant surgery places the lateral incision above the location of the marginal mandibular branch of the facial nerve.
2) Medpor jaw implants can be effectively removed through a transcutaneous approach with a lower risk of implant replacement infection.
3) The transcutaneous jaw implant approach requires splitting the masseter muscle sling which must be reapproximated during closure.
Dr. Barry Eppley
Indianapolis, Indiana