Background: Shoulder narrowing surgery is a conceptually ‘simple’ aesthetic concept. Remove a piece of the clavicle, pull the two ends together and the shoulder will appear less wide. While from a conceptual standpoint this is true, actually doing it through limited surgical access from a favorable incision location successfully is a bigger surgical challenge that it initially seems. It is not, as it is often compared, like a clavicle fracture repair at all.
In clavicle fracture repairs the incisions used are far greater in length and placed to where it provides the best visibility to most successfully fix the problem. But of equal relevance is the now inwardly pulled shoulder from the loss of clavicle length only needs to be brought back out to its original length and then stabilized. Besides the obvious incisional length and location differences, shortening the clavicle requires pulling the shoulder inwards against the natural weight of the shoulder girdle tissues…a far different mechanical challenge in which the shoulder is moved inward to a position in which it has never been.
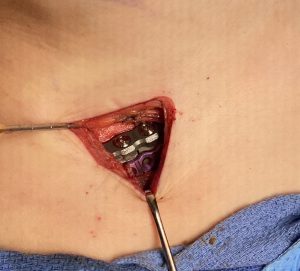
While technically challenging in any patient, larger and/or thicker tissue patients compound that challenge. The greatest the thickness of the tissues that overly the clavicle the more difficult it is to work through the identical length incision…meaning the incision length does not change even though the patient’s anatomy does. How cdalleningn it will be can be seen beforehand depending upon how much clavicle show the patient has.




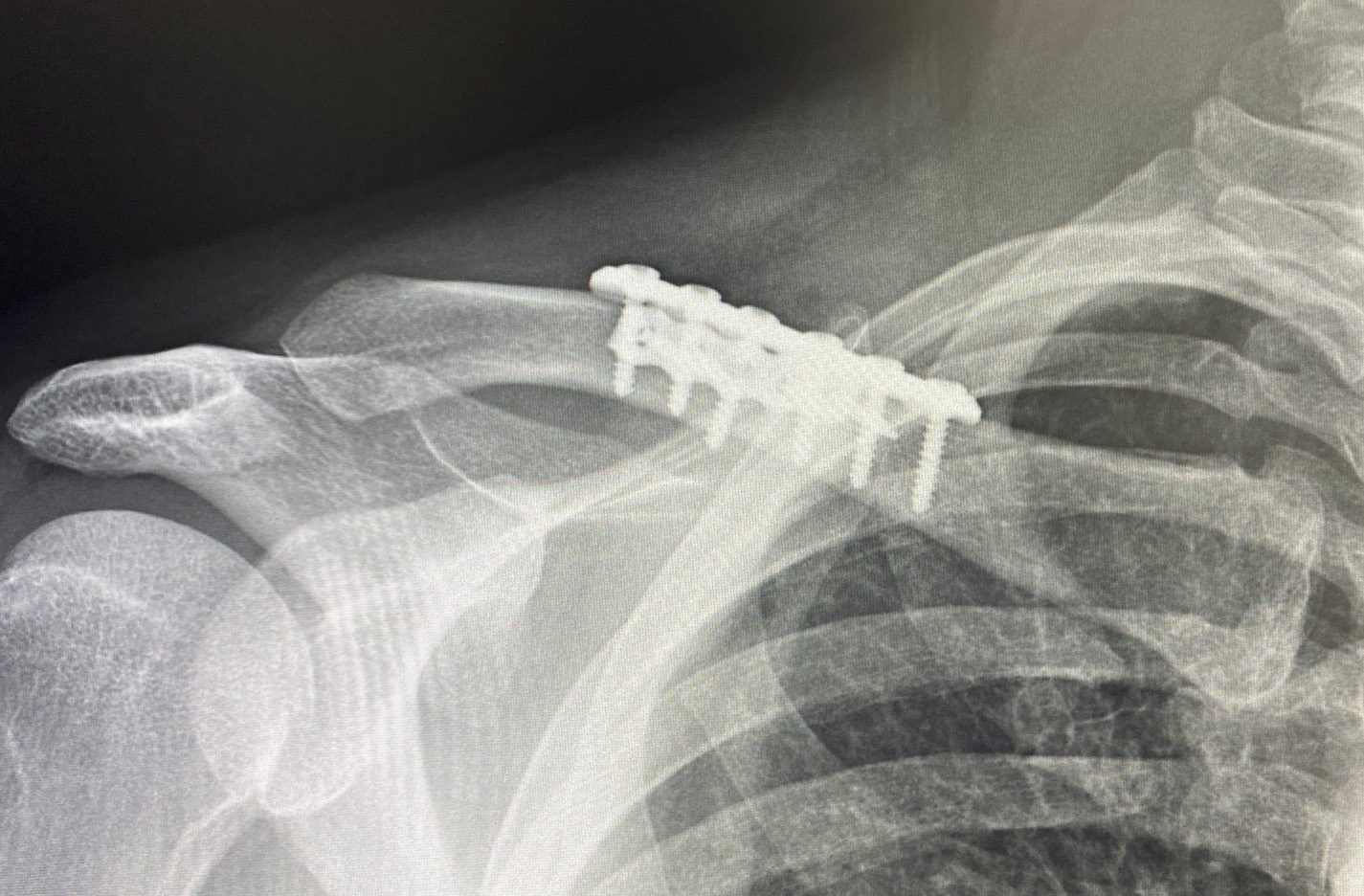
Besides the challenges to which surgical access is exposed in the presence of lack of any clavicle show, there is also the weight or heaviness of the shoulder in such patients. This poses expected technical difficulties in bringing in the shoulder and holding it in good alignment with the stable inner clavicle segment to apply the fixation. (this requires two people to do it) But it also illustrates the stress the plate and screw fixation is under to maintain the alignment of the two bone segments as it heals. This is definitely not the same as re-establishing clavicle length in fracture repair. While in clavicle fracture repair orthopedic surgeons are very reticent to ever apply more than one plate for understandable fear of impeding bone healing, the clavicle in that situation is much more devascularized from the injury and the dissection needed for long plate applications. Shorter plate application in clavicle osteotomies and the increased stress of an unnatural new shoulder position make the use of double plate fixation more secure particularly in the heavier thick tissue shoulder patient.
Case Highlights:
1) Lack of clavicle show portends a deep dissection to get to the bone through the limited supraclavicular skin incision used in shoulder narrowing surgery. (clavicle reduction osteotomies)
2) Fortunately the supraclavicular incision provides a mobile window which can be moved around to accomplish the work needed on the much greater length of the clavicle than the limited linear incisional length would suggest is possible.
3) The hardest part in patients with larger shoulder girdle mass is being able to move the entire shoulder inward and holding it in place to stabilize it with plates and screws.
Dr. Barry Eppley
Indianapolis, Indiana