Background: One of the smaller and least recognized areas of facial augmentation is the central nasal region. Reasons for augmenting the base of the nose are for general midface retrusion or flattening but can also be done to improve the nasolabial angle/upper lip projection or to soften deeper nasolabial folds at the alara-facial junction. Premaxillary and paranasal augmentation historically was introduced as an adjunct to rhinoplasty often in Asian patients. But today it is used in a wide variety of patients and the potential aesthetic benefits of this area of facial augmentation has developed increased awareness due to the popularity of injectable fillers.
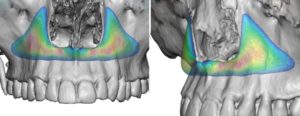
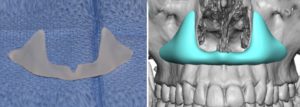
Premaxillary and paranasal implant styles have been around for decades but have been dominated by one standard implant design, the pyriform implant. This is a combined premaxillary-paranasal implant design that encircles the lower pyriform aperture or bone that surrounds the nasal cavity. Centrally it crosses the anterior nasal spine and extends laterally up along the bone staying medial to the canine fossa. Externally its effects are to push out the based of the nose from the columella centrally to the attachments of the nostrils laterally. While this is not a complex implant design per se, subtle variations in its design can determine how it feels externally to the patient. (or whether they can feel it at all)
When augmenting the bony pyriform aperture it is important to recognize that the pyriform aperture has a concave surface laterally and a more pointed convexity centrally. Careful inspection of the anatomy shows that even in patients with good nasal base projection these surface contours remain the same. Thus any premaxillary-paranasal implant design should have edging that flows smoothly into the surrounding bone to avoid creating an unnatural ‘bump effect’.


Case Highlights:
1) Nasal base augmentation consists of either lateral (paranasal) or central (premaxillary) zones or a combination of both
2) Successful designs for premaxillary and paranasal implants is to have feathered edges that blend into the surrounding bone.
3) A custom premaxillary-paranasal implant can be placed intaorally with a frenum-sparing incisional approach.
Dr. Barry Eppley
Indianapolis, Indiana






