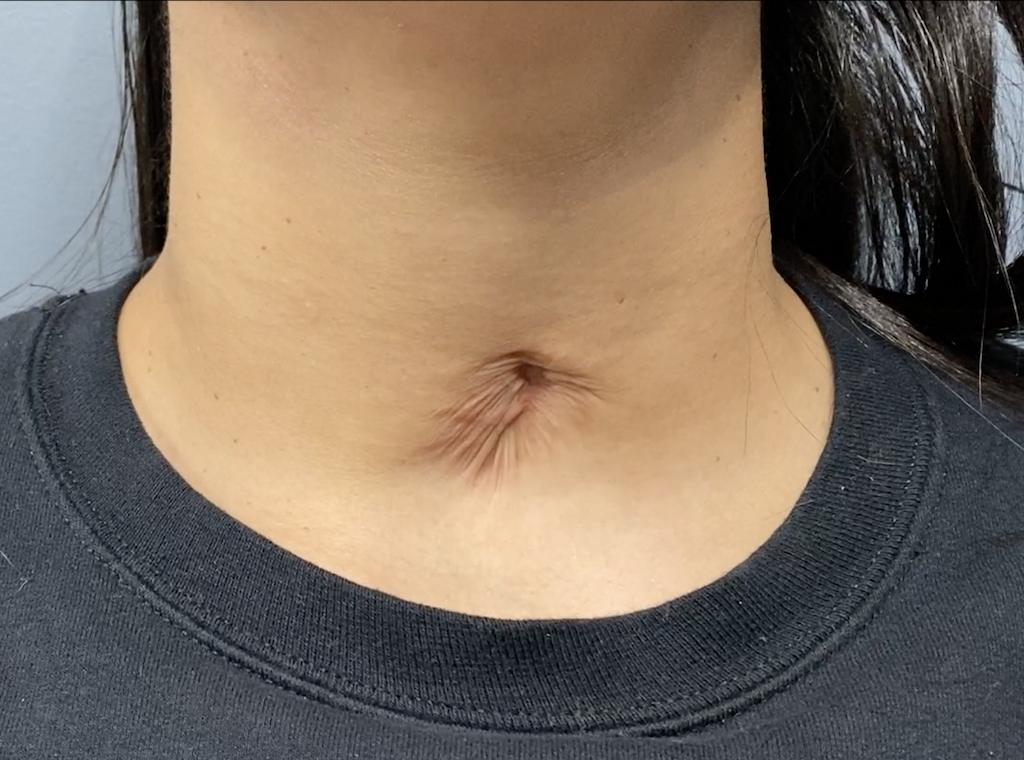
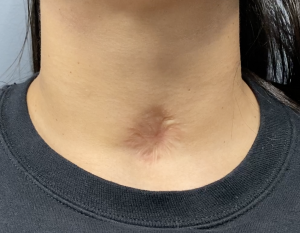
Background: A tracheostomy is an urgent surgical procedure to establish a payment airway below the level of the thyroid cartilage and vocal cords. How long a tracheostomy stays is variable based on the reason it was initially inserted but eventually most are removed. When the tracheostomy is removed the resultant wound its allowed to heal in on its own. While it usually heals without a fistula (residual hole into the trachea) it always heals with a greater indentation above the sternal notch that originally exists and the scarred skin is usually fairly wide.
The placement of a tracheostomy tube, no matter how long it is in place, usually results in a soft tissue deficiency when it is removed. The longer it is in the greater the soft tissue loss of fat is between the skin and the trachea… not to mention the persistent separation of the sternothyroid muscles which contributes to the depth of the healed indentation. This is why trach scars are usually more indented than the normal suprasternal contour depression. The significance of the soft tissue loss is most seen when a visible retraction of the scar occurs when swallowing, indicating a direct adhesion of the skin to the trachea.
While many trach scar revisions can be treated by scar excision and skin flap coverage over the defect. When scar reatraction occurs with swelling the softy tissue defect is greater and must be addressed for an improved trach scar appearance.



In this more uncommon trach scar indentation, a tube placed at a very young age and in place for a few years during early development, is going to cause a more severe permanent scar indentation than occur in many other trach scars. But when the scar retracts with swallowing this indicates a direct skin adhesion to the trachea with no intervening soft tissue. In this type of trach scar revision soft tissue replacement is needed and a small dermal-fat graft is ideal for the size of the created defect from the skin excision/release.
Key Points:
1) A deep trach indentation with scar retraction when swallowing represents a soft tissue deficiency.
2) Removal of the scarred skin in a trach scar revision provides a release of the adhesion and establishes the volume of soft tissue loss.
3) A dermal-fat graft is the needed soft tissue volume replacement in the recontouring of a deep trach scar indentation with retraction.
Dr. Barry Eppley
World-Renowned Plastic Surgeon