Background: Make chest enlargement or gynecomastia has a variety of different presentations. How much breast tissue enlargement, the amount of loose skin on the chest wall and the position of the nipple all influence the type of gynecomastia reduction technique that will be used.
Most gynecomastia techniques employ either direct excision by an areolar incision, liposuction or some combination of both. While effective for most young patients, the older gynecomastia patient often has one anatomic component that may change the surgical approach….nipple sagging or ptosis. This is defined very similarly to that of the female breast patient through the relationship of the nipple to the inframammary fold. And just like in the female when the nipple sits at or below the inframammary fold, no change in the breast/chest wall volume is going to make the nipple sit higher and look less ptotic.
In the older male gynecomastia patient, the nipples are often in a ptotic position. Even if the chest enlargement is not big, the nipple and its underlying breast tissue hand off the chest wall….creating an unattractive ‘man boob’. No amount of pectoral muscle development is going to lift the nipple up. And, in fact, significant pectoral muscle hypertrophy will make it look even worse by accentuating the overhang.



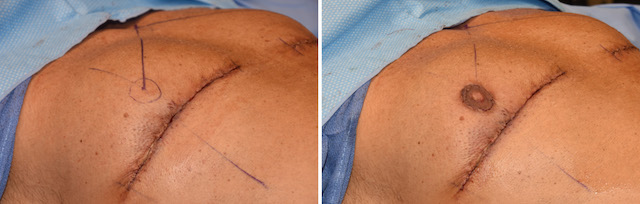
For significant nipple ptosis in the older gynecomastia patient, the nipple is going to have to be relocated. While free nipple grafting is always an option, there is the risk of depigmentation or portions of the nipple graft not surviving. Transposition of the nipple by keeping it attached to the chest tissues avoids these risks or at least significantly decreases them.
In solving the nipple overhang issue the trade-off is an inframammary scar. As long as it does not get into the sternum medially or extend to far out laterally, this is usually an acceptable aesthetic trade-off.
Case Highlights:
1) When nipple ptosis occurs in older gynecomastia males, no form of soft tissue reduction will elevate the nipples into a better or less ptotic position on the chest wall.
2) In such gynecomastia reductions the nipples need to be directly elevated by transposition or free nipple grafting.
3) In nipple transpositions setting its new elevated position. must avoid over correction or too high of a chest wall position.
Dr. Barry Eppley
Indianapolis, Indiana