Background: There are a variety of medical complications that can occur of any facial implant, including chin implants, of which the most feared is infection. When infection occurs around a chin implant, its salvage by any variety of maneuvers is frequently unsuccessful. Removal of the infected implant is always the definitive treatment. Re-implantation at a later date will usually be successful.
The other significant medical complication of facial implants is exposure. This can occur when the implant is chronically infected and the tissues erode between the implant and the incision. The line of dissection from the incision to the pocket offers the least path of resistance for tissue breakdown. Implant exposure can also occur in a non-infected implant in which it has applied too much pressure on the overlying tissues. This can occur from an implant that is too large, a tissue pocket that is too close to the incision or a combination of both.
But regardless of the reason for implant exposure the compromised tissues around the implant are rarely satisfactory for efforts at attempts at reclosure. Nor will the tissues granulate over the implant’s surface and create a secondary intention healing regardless of the material’s composition. The implant is going to have to be removed. But the interesting future question is whether the tissues will be good enough int the future to allow for the potential for re-implantataion.




When treating an implant exposure which requires its removal, thought needs to be given to what the tissues will be like if reimplantation is done later. When the quality of the tissues are poor/deficient the placement of an enbloc fat graft can help improve tissue quality and quantity.
Case Highlights:
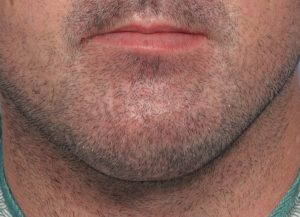
1) Chronic infections in chin implants often result in loss of soft tissue which can leave the implant exposed whether from an intraoral mucosal or a submental skin incisional placement.
2) Removal of the infected chin implant and all hardware is the key to infection resolution but not to the resultant soft tissue defect.
3) Immediate reconstruction with an inlay fat graft can help restore soft tissue volume loss which would be needed if secondary implant augmentation is to be attempted.
Dr. Barry Eppley
Indianapolis, Indiana