Background: Medpor or porous polyethylene is a common facial implant material. Its primary biologic feature as an implant is that is surface porosity permits soft tissue attachments/ingrowth. While this is perceived by some as a material benefit it become a major material liability should any form of revision or removal of the implant be needed. These soft tissue attachments are tenacious and removal can be extremely difficult. Injury to surrounding nerves and blood vessels, if in the vicinity, can be a real risk. The risk of implant removal can be greater than implant insertion which is not a good material feature.
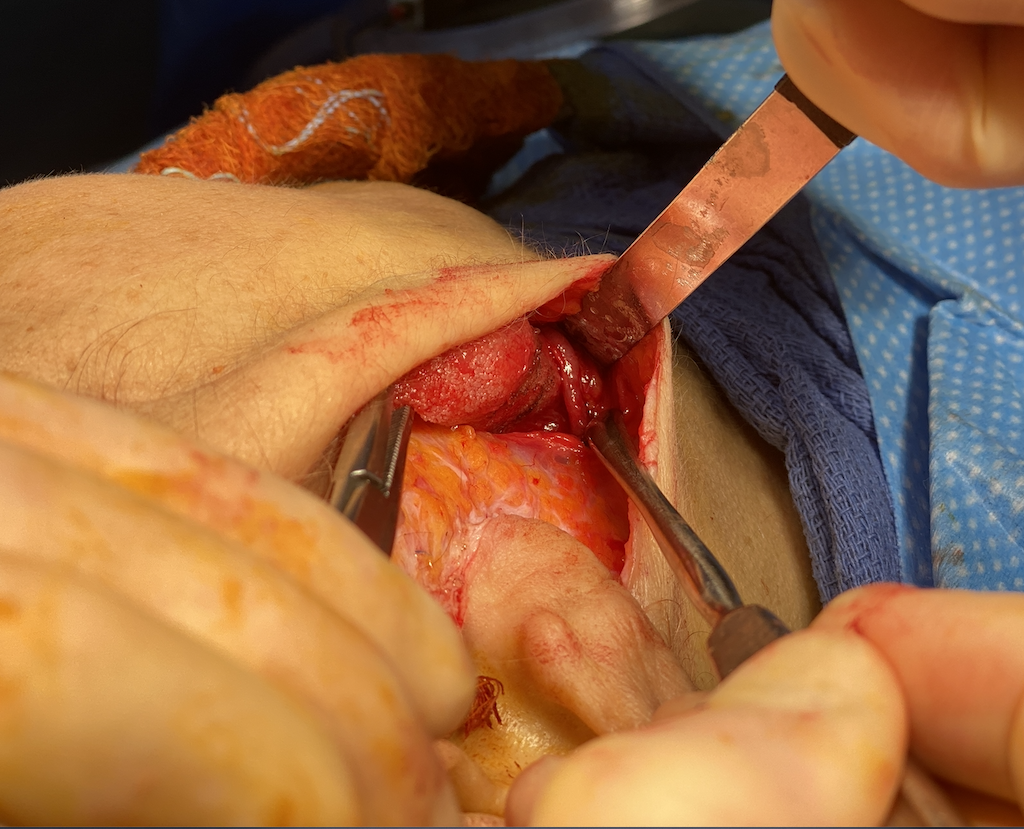
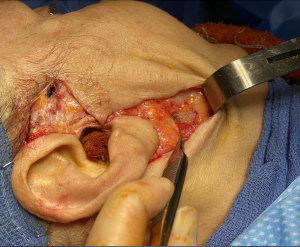
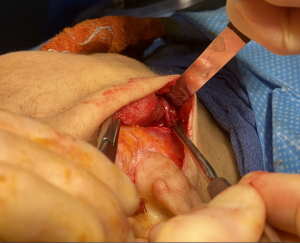
Having removed hundreds of Medpor facial implants none are more challenging than those along the jawline, particularly the jaw angle region. Besides the difficulty working way back in the posterior region of the mouth the soft tissue attachments of the masseter muscle are very adherent. But what really makes this area for Medpor implant removal difficult is that many of the standard jaw angle implants are designed to wrap around the inferior border to create a vertical lengthening effect. While this is a sound design and has good aesthetic benefit it also complicates removal due to the limited intraoral exposure. But one additional variable increases the risk of Medpor jaw angle implant removals…the adherence of the facial artery to the implant as it crosses up from the neck over the implant into the face. I have more than once partially transected this artery during their removals and, while not life threatening, can be difficult to get the bleeding under control.
An alternative approach to Medpor jaw angle implants removal is through a facelift which approaches implant removal from a different and more favorable direction.



Case Highlights:
1) Women more so than men may find that a jaw angle implant has a masculinizing effect.
2) Through a facelift a direct approach from the implant’s posterior surface can be done and the recovery improved by avoiding a healed intraoral incision..
3) A facelift approach provides better visualization of the crossing facial artery which should injury occur can be more easily controlled.
Dr. Barry Eppley
Indianapolis, Indiana