Background: The vast majority of temporomandibular joint (TMJ) dysfunction/pain is extra capsular or outside of the joint. It is more related to the attached muscles and ligaments that work around the joint. But there are some cases where true intracapsular involvement occurs particularly when the lower jaw has been exposed trauma. The condyle of the joint may be forcibly driven upward into the glenoid fossa causing bleeding into the joint and even meniscal tears. Or the condyle may be rapidly distracted away from the joint space stretching the surrounding capsule.
Either way, the small TM joint space can develop adhesions/scarring that prohibits smooth meniscocondylar movements that are needed for unobstructed and pain free mouth opening. The affected TMJ may lose the ability to translate out of the fossa (fixed dislocation) or may do so with a symptomatic click from compression of the meniscus. (reciprocal dislocation) These are indications for a TMJ arthroplasty procedure to free up the scarred meniscus and capsule as well as to reduce the bony eminence to make it easier for the meniscus to have a more normal gliding motion.
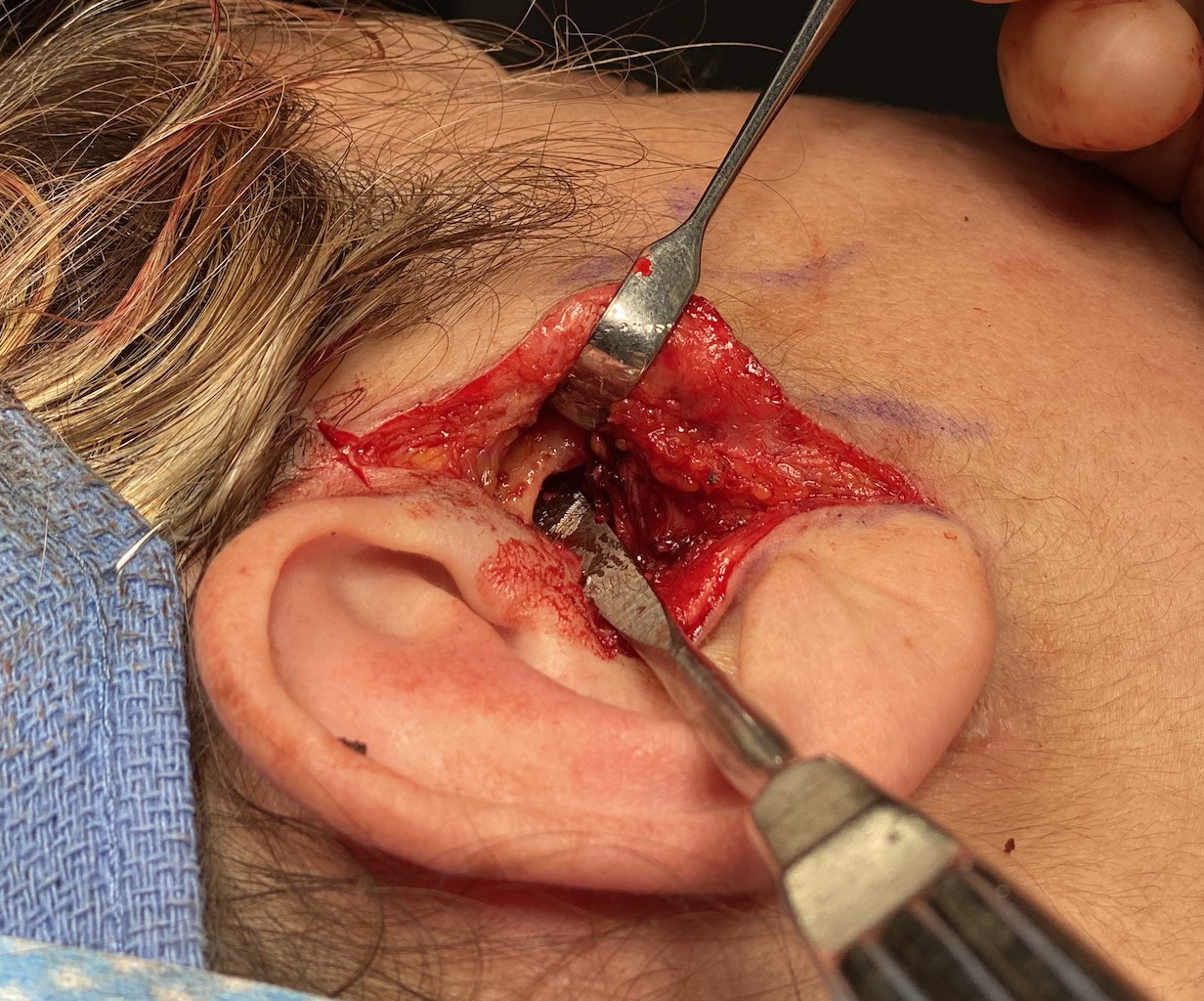
One can have a debate about whether a TMJ arthroplasty should be done through an arthroscopic or open approach. But in cases of fixed meniscal dislocations I think the open approach offers a more complete treatment of the involved tissues.
Case Study: This female had a surfboard injury to the right side of her face resulting in multiple traumatic injuries. One of them was right sided facial pain that centered around the ear and TMJ. She had difficulty opening her mouth with jaw deviation to the right side and limited condylar translation. The left TMJ had normal condylar translation and was pain free.


Once the articular eminence was fully exposed it was reduced by a high speed handpiece to remove most of its prominence, making it easier for the meniscus to move back and forth.

Case Highlights:
1) Fixed meniscal dislocations of the TMJ can occur traumatic injuries to the face that either compress or distract the condyle.
2) An open TMJ arthroplasty allows for maximal release of meniscal adhesions/scarring and creating an increased joint space for its movement.
3) To prevent postoperative capsular tightness of the joint, fat grafts are used to introduce new tissue rather than closing/tightening down the capsule.
Dr. Barry Eppley
Indianapolis, Indiana