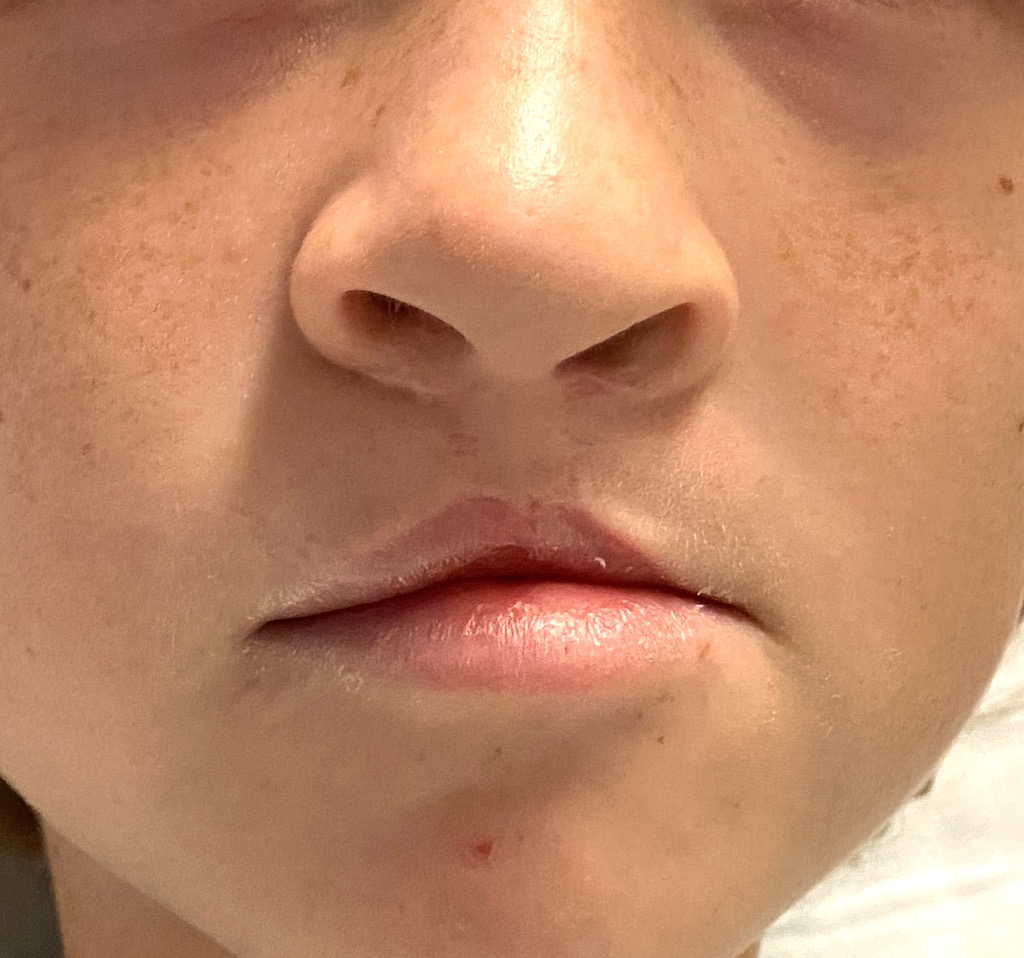
Background: One of the most common congenital facial deformities is that of cleft lip and palate. While occurring in a diverse spectrum of presentations, at the most simplistic level cleft facial deformities can be divided into unilateral and bilateral clefts. What separates the bilateral cleft from unilateral ones is that the central lip segment (prolabium) is smaller/thinner and the nasal tip is underdeveloped with wider nostrils. Ultimately the more extensive involvement of the bilateral cleft poses longer term reconstructive challenges.
Like all clefts the bilateral cleft reconstruction begins with an initial primary repair done in the first year of life in which the lip is put back together on both sides which also pulls in the flared nostrils as well. While other cleft-related issues will be managed in the more immediate years thereafter (cleft plate repair, alveolar bone grafting) the external appearance of the lip and nose will not again be operated on until past puberty as a teenager when facial growth has slowed down and the face is more developed.
But between the long time period between the primary repair and the teenage years the psychological sequelae to the child of the bilateral cleft deformity remains. Despite the best primary repair the bilateral cleft deformity represents a lack of normal tissue volume and growth makes this more apparent. While the definitive revisions of the bilateral cleft is ideally done when the tissues are larger and future facial growth is more limited, there is a role for helpful revisions in the interim.




Many cleft patients undergo multiple revisions of their cleft lip and nose deformities after the primary lip repair. To some degree the problem is chased until growth is complete. Revisions are often done before facial growth is complete particularly when the child is bothered by their appearance or is being teased for it. The key is to do such revisions that provide impr0vemen but did not add to the scar burden or make further revisions when they are older more challenging or complicated.
Case Highlights:
1) The bilateral cleft deformity, despite excellent primary repairs, will often have a short central lip segment and widened nostrils.
2) While a definitive bilateral cleft lip and nasal revision may await the teenage years, younger patients are still subject to ridicule because of their orofacial appearance.
3) An early bilateral cleft revisional approach of internal V-Y mucosal advancement with fat grafts and internal nostril wedge narrowing offers improvements that does not adversely affect any future revisional surgery efforts.
Dr. Barry Eppley
Indianapolis, Indiana