Background: Skull defects can be reconstructed by a variety of methods from implants to grafts. If the patient prefers an autologous method then a bone graft is needed. Technically a bone graft could be obtained from a tissue bank (cadaveric or allograft bone) or from the patient themselves. But for a truly autologous bone graft donor sites include the skull (regional donor site) vs rib. (distant donor site) There are advantages and disadvantages to either donor site and it is really a patient’s choice. But for small skull defects keeping the donor site close to the recipient site offers incisional efficiency.
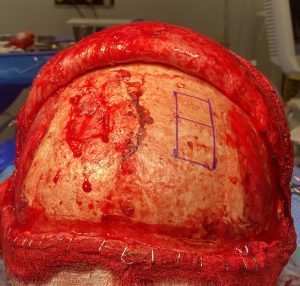
When harvesting a bone graft from the skull there are three consideration to be made. How much bone is needed (size of the graft), what technique will be used to harvest it and the management of the contour defect left from the harvest. In smaller skull defects an external split-thickness harvest method can be used which minimizes any significant residual contour defects.
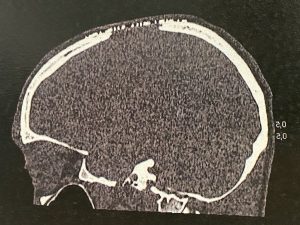
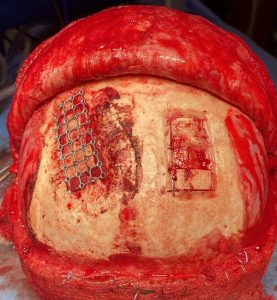
While she had no postoperative problems with the skull defect reconstruction she desired to have it reconstructed by bone. She preferred bone up against her brain as opposed to metal.
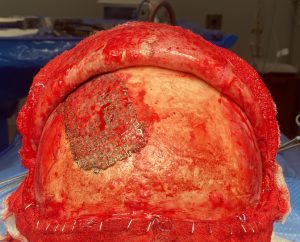



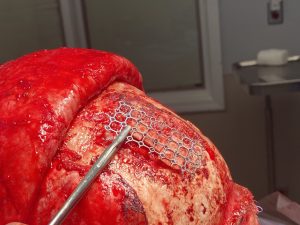
In harvesting split-thickness cranial bone grafts there are two techniques. One method is to do a craniotomy, take the full thickness bone and split it into inner and outer layers and then use one of the pieces to reconstruct the skull defect. This is a good technique if the bone graft needed is very large. In smaller bone graft harvests removing the outer table of bone by splitting it in place is preferred. It is technically more challenging but spares doing a craniotomy.
Case Highlights:
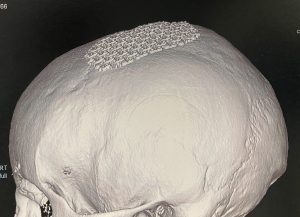
1) A mesh metal plate is not an ideal method for covering a full thickness skull defect as it allows significant soft tissue ingrowth and makes removal difficult.
2) Autologous reconstruction of a fill-thickness skull defect requires a bone graft.
3) Split-thickness cranial bone can be used to reconstruct a skull defect and can be done by a non-craniotomy technique.
Dr. Barry Eppley
World-Renowned Plastic Surgeon