Background: The chin implant is viewed as a simple surgery with no significant anatomic issues for its placement. But this often viewed concept is inaccurate as it fails to appreciate that an important element of making the implant pocket is release of some or all of the osteoligamentous attachments in making the suboperosteal pocket. If not adequately released implant malpositon will occur when using any winged chin implant style. (extended anatomic designs)
While release of the ligaments are a necessity for implant placement there are potentially adverse sequelae should the implant ever be removed. Contrary to popular perception of many surgeons the chin is not simply going to shrink back down and return to normal. It can’t as the ligaments can not reattach once they have been released. The capsule on the outer surface of the implant on the tissue side slides off the underlying capsule of the bone once the implant spacer is removed between the two. This causes some degree of chin road sagging/excess. This can be very minor and aesthetically irrelevant to the patient. Or it can be more significant and problematic to them.
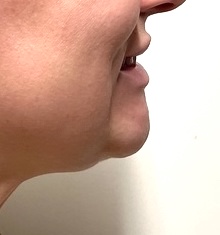
Soft tissue chin pad excess after implant removal is typically most pronounced when smiling. This causes a new/unnatural roll under the chin and, in more significant cases, may display a pulldown of the chin pad. (hyperdynamic chin pad ptosis) The only effective treatment is removal of a portion of the chin pad and tightening it under the chin bone. Techniques such as intraoral suspensions and chin pad liposuction will universally fail to provide any improvement.



Case Highlights:
1) The soft tissue chin pad after implant removal may not return to its preoperative shape due to loss of its osteoligamentous attachments
2) Soft tissue chin pad excess can only be improved by an excisional technique.
3) One of the keys to soft tissue chin pad excision is to prevent its lateral extent from crossing the mouth corner-jawline triangle border.
Dr. Barry Eppley
World-Renowned Plastic Surgeon