Background: Silicone injections to the genitals (penis and scrotum) is a known method for aesthetic enlargement of these genital structures. While not an FDA-approved procedure or injection material it is often done outside the U.S.. Such silicone injections create their effect as the material is non-resorbable. The body has no known enzymes to break the material down and the silicone molecules are too large to be removed by macrophages. Since silicone is a foreign material the body tolerates it by an encapsulation process. This encapsulation is the body’s method of isolating a material that it does not see as itself…but will tolerate it by keeping it isolated from then rest of the body.
The most common problem with silicone injections are irregularities under the skin due to the encapsulation process. These are benign albeit aesthetically bothersome if significant. In general, despite silicone being a foreign substance and having a very checkered history, many silicone injected patients do just fine years later. But there is a subset of silicone injected patients that develop inflammatory responses to the material. There are usually delayed and of a chronic nature rather than an acute reaction that develops right after the injections. What tips the balance between tolerance and developing an immune response to the material is not precise known particularly when the reaction does not develop until years later.
When an immunologic response develops to injected silicone steroids, either given systemically or being injected locally, will usually quell the inflammatory response in the short term. In the long term, however, removal of the injected silicone material provides the definitive cure. But excision of silicone is not easy and often not possible in the face without major aesthetic tradeoffs. But in the body excision of silicone, most commonly done in the buttocks, is more effective although not without some aesthetic liabilities. In the scrotum the decision is whether the silicone can be excised while preserving the testicles or whether testicle removal is necessary.
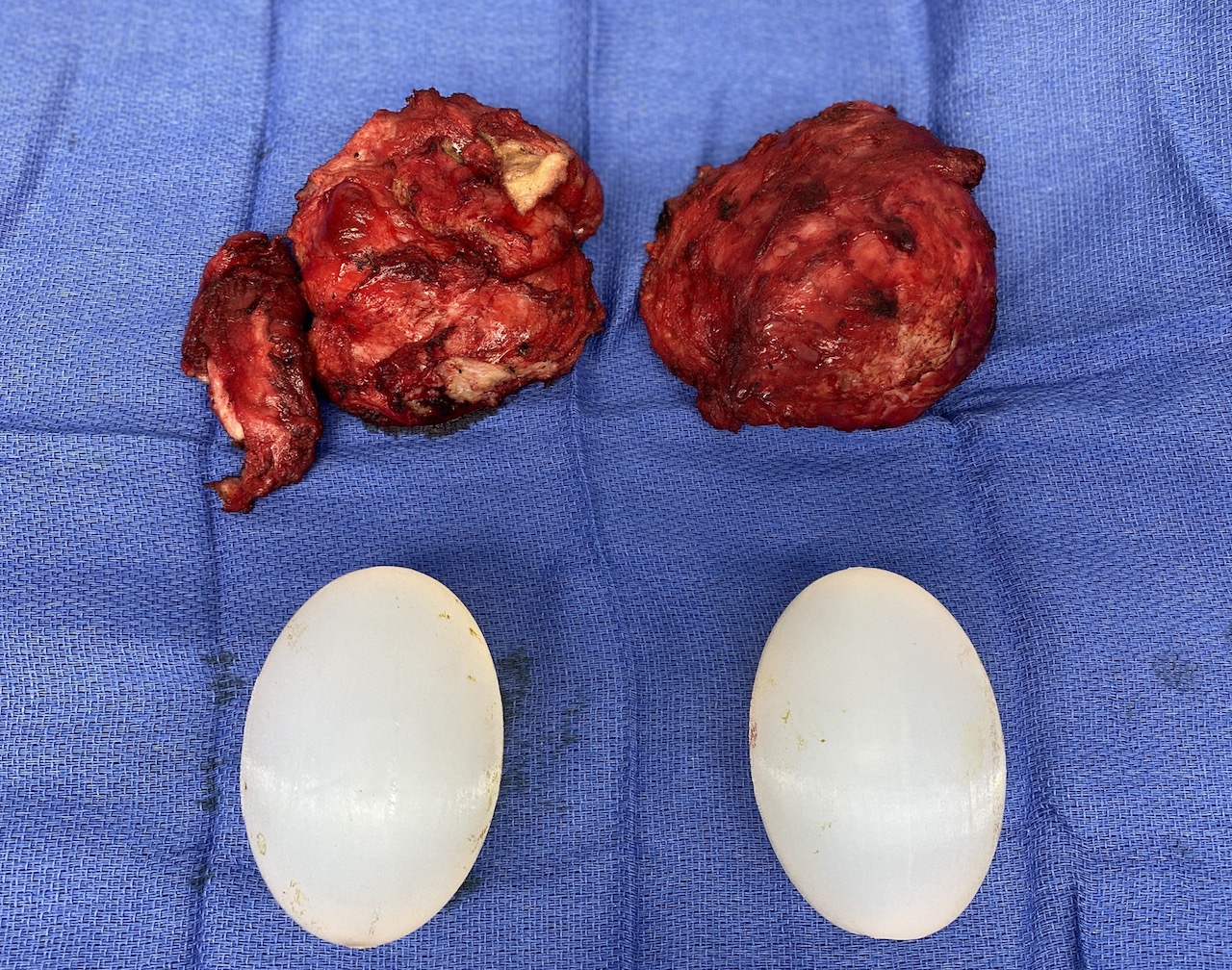
Case Study: This male had penile and scrotal silicone injections done 12 years previously. He never developed any problem with the injections until he contracted COVID. Thereafter the scrotum developed a chronic inflammatory reaction which was partially suppressed by oral steriods. Most of the silicone injections appeared to be around the testicles, which were naturally large, but now even larger. Since he was not interested in having children and was already taking testosterone supplementation the best way to ensure that the silicone was completely removed was to remove both testicles. Since he wanted to maintain his same scrotal size, he decided for 8.5cm testicle implant replacements.




One very interesting aspect of this case study is that the patient had silicone injections for over a decade and never had a problem. Contracting COVID somehow changed his immune system response to it. Another unusual COVID sequelae that currently defies explanation.

Case Highlights:
1) Silicone injections to the scrotum can eventually develop chronic inflammatory reactions…in this case due to COVID.
2) The most assured method of resolving the inflammation from a silicone injected scrotum with extensive testicle involvement is to remove them.
3) XL testicle implant replacements can be made extra softy by the incorporating a small hollow inner chamber.
Dr. Barry Eppley
World-Renowned Plastic Surgeon