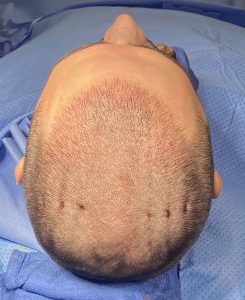
Background: While there are a variety of pathologic conditions that can affect the scalp none is more unusual that cutis verticis gyrata. (C VG) While most people have seen someone so affected few realize that it is an actual pathologic problem. Appearing as wrinkles on the head is why is called gyrata being similar to the appearance of the surface of the brain. In most patients these wrinkle lines are not random but rather vertical running from front to back. (hence the term verticis or vertical) There can be single or multiple lines in the scalp and they can be slight in depth or very deep.
CVG is not present at birth and develops later in life. What causes it is not known although it appears somewhat similar to a facial condition known as linear scleroderma (LS) in terms of appearance, timing of onset and progression The difference is that LS is an atrophic condition of the skin and subcutaneous fat along vertical lines the following the path of the trigeminal nerve. CVG is a fibrosis/contracture of the skin and subcutaneous fat that, while usually vertical, is random in its scalp location although most occur on the top and sides of the head. Usually they occur one both sides of the head and are often perfectly symmetrical. (e.g., if there are three lines on one side there are three lines on the opposite side)
The historic method of treating CVG is excision of the indented scalp lines. While such excision is the only effective treatment for very deep V-shaped CVG lines, the scar tradeoff is less deep lines may not be acceptable or impractical when multiple lines are close together. An alternative treatment is release and fat grafting in the properly selected patient..



Case Highlights:
1) CVG appears as linear fibrotic lines in the hair bearing part of the scalp whose etiology is unknown.
2) One treatment option its subcuticular release with injection fat grafting using a specialized instrument to do so.
3) It is not yet known how effective this treatment is for CVG or whether it will stop its progression but it is a benign treatment using the patient’s own tissues so there is little downside to it.
Dr. Barry Eppley
Indianapolis, Indiana






