Jaw angle implants, whether they be standard or part of a custom jawline implant design, require an intraoral incision for placement. This incision is way back in the mouth opposite the second or third molars either in the vestibule or slightly up on the cheek mucosa. Lying directly under the incision at some depth from the surface is the implant. Usually a thick layer of soft tissue exists, consisting of mucosa and muscle, which heals and separates the implant from any intraoral contamination.
Such a posterior vestibular incision is exposed to the forces of chewing and food debris. As a result there is always the potential for wound breakdown and implant exposure to intraoral fluids and subsequent implant infection. This risk is increased in revisional jaw angle implant surgery where the quality of the incisional tissues lessens due to formation of scar tissue. The vestibule deepens and the integrity of secondary wound closure may be compromised.
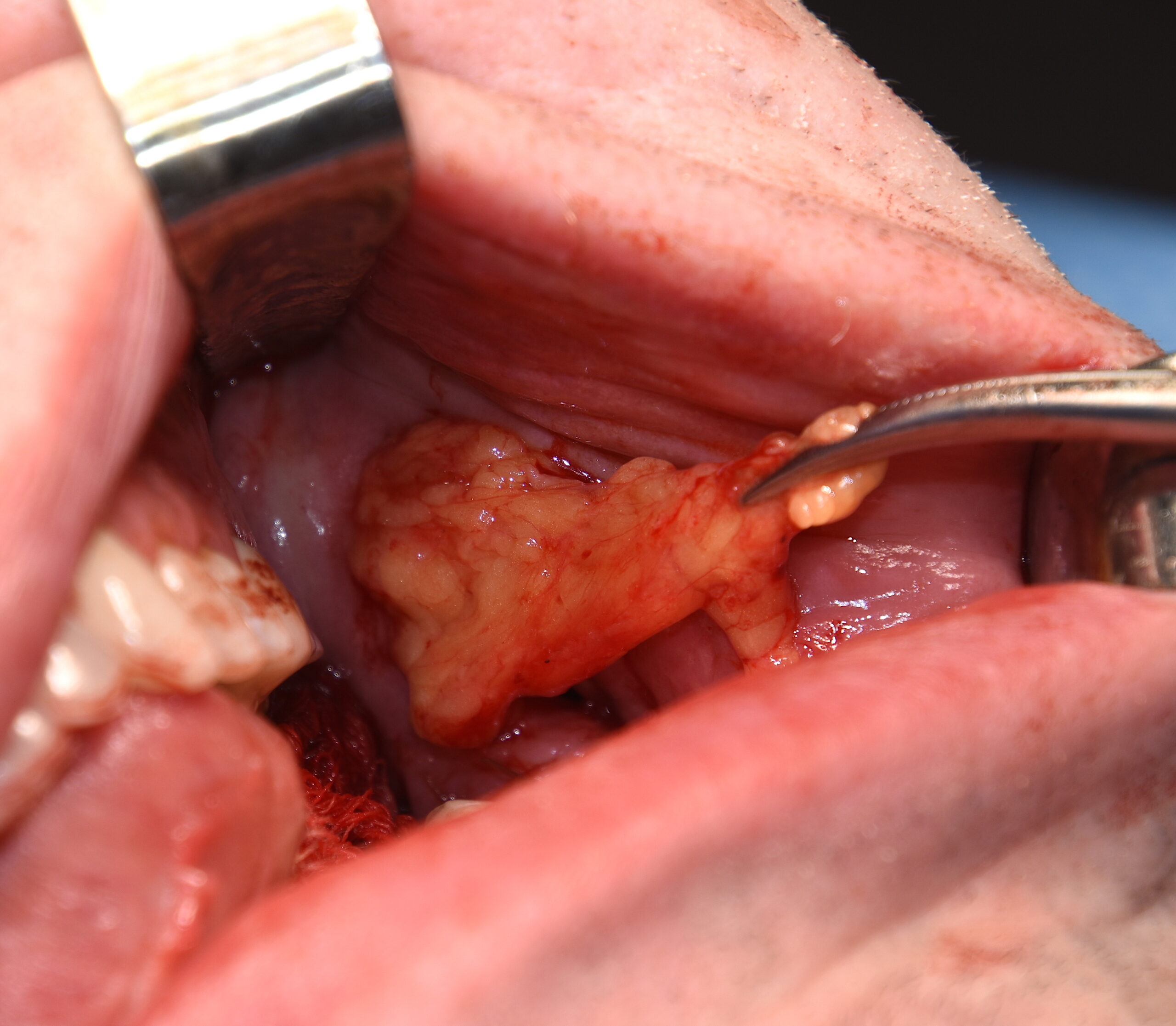
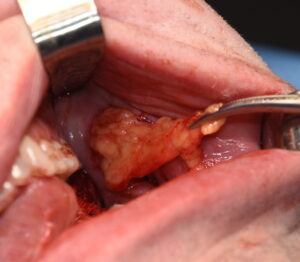
A useful technique, when either the incisional tissues are thin/compromised or wound dehiscence has occurred, is a pedicle buccal flap transposition. The key to improving the chances of a compromised posterior intraoral incision to satisfactory heal and salvage an underling implant is the recruitment of new tissue into the wound. The best tissue for this and one that is in close proximity is the buccal fat pad.


Dr. Barry Eppley
Indianapolis, Indiana