For major nasal augmentations the options come to using a rib graft or an implant to achieve it. Each augmentation method has their own advantages and disadvantages and one isn’t necessarily better than the other. Each patient situation must be assessed on an individual basis in terms of amount of augmentation needed and the patient’s risk vs scar tolerance.
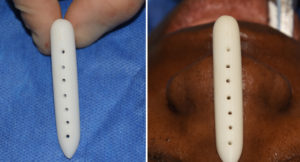
The major advantages of a nasal implant are obvious… no donor harvest scar, less operating and recovery time and an assured straight form with a guaranteed augmentation effect based on its dimensions. But one of its known side effects is that the implant can become deviated or misaligned. This risk is greater in silicone nasal implants because they have a smooth surface and contracture around them over time can cause their position to change. This is because they do not integrate into the surrounding tissue and are more prone to deformational forces. Other types of nasal implants, such as porous polyethylene and ePTFE, allow for tissue adherence and are less likely to undergo secondary positional displacement.

Dr. Barry Eppley
Indianapolis, Indiana


