Jaw angle implants are a common form of aesthetic facial augmentation. They are unique from some other types of facial implants because of their need for bilateral placement as well as accessing the very remote jaw angle area intraorally. As a result jaw angle implant malposition is not rare and, given that many patients have natural bony jaw angle asymmetry, it may almost be considered the norm.
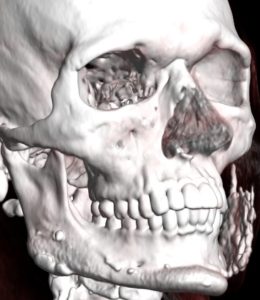
Most cases of jaw angle implant asymmetry can be improved by the same method by which it was placed from an intraoral approach. One can expect to run into bony overgrowth onto the implant almost always from the superior aspect of the implant. This will necessitate bone removal and uncovering of the implant which will present some technical challenges. This is one reason why a preoperative 3-D CT scan should almost always be done, to not only assess the actual position of the implants but also to avoid any ‘surprises’ during surgery.
An alternative approach to intraoral jaw angle implant repositioning is an external one. This is where a small incision is made directly near the jaw angle area and is known as a direct transcutaneous approach. This has numerous advantages including avoiding the longer recovery from an intraoral approach, a lowered risk of infection, and more direct visualization of the working end of the jaw angle implant (which in my experience leads to a better chance of a more ideal implant repositioning).

The scar from the transcutaneous jaw angle implant approach heals exceptionally well particularly in the male patient. The presence of beard skin, whether the patient regularly shaves or not, accounts for the excellent scar outcome. Equally importantly, visualizing the working end of the implant over the bony area in which it is to be placed, provides the best opportunity for secondary implant repositioning.
Dr. Barry Eppley
World-Renowned Plastic Surgeon




